Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Antiphospholipid syndrome (APS) is a systemic autoimmune disorder characterized by thrombotic events and obstetric complications. While macrovascular and microvascular manifestations have been increasingly acknowledged—particularly with the inclusion of microvascular lesions in the 2023 ACR/EULAR classification criteria—arterial stenosis within the central nervous system (CNS) remains insufficiently recognized. This study aimed to systematically evaluate the prevalence, imaging features, and possible pathophysiological mechanisms of intracranial arterial stenosis in patients with APS.
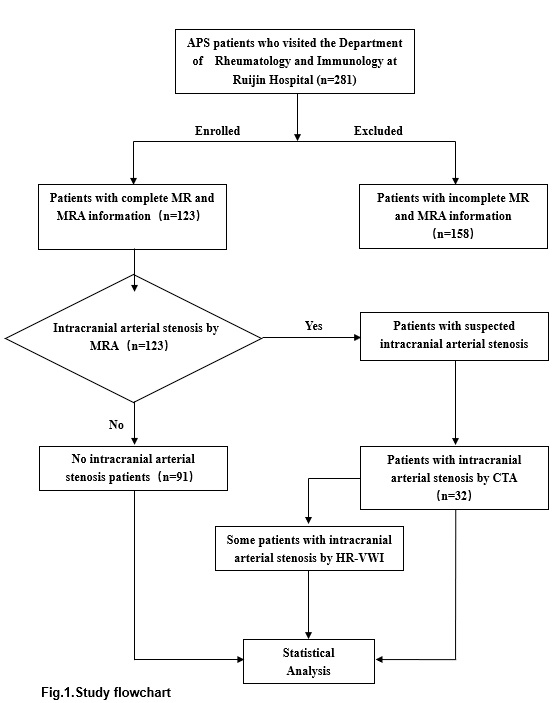
Methods: We prospectively enrolled 123 APS patients meeting the 2023 ACR/EULAR classification criteria. All participants underwent cerebrovascular screening using magnetic resonance angiography (MRA) to detect potential abnormalities. Patients with suspected arterial stenosis on MRA subsequently underwent computed tomography angiography (CTA) for definitive anatomical confirmation. In those with CTA-confirmed intracranial stenosis, high-resolution magnetic resonance vessel wall imaging (HR-VWI) was performed to assess wall morphology, contrast enhancement, and features suggestive of inflammatory vasculopathy (Fig.1).
Results: Among the 123 APS patients screened, MRA revealed cerebrovascular abnormalities in 76 patients (61.79%), including 32 patients (26.0%) with confirmed intracranial arterial stenosis with CTA. Other observed MRA findings included suspected stenosis (2.44%), arterial slenderness (18.70%), protrusion shadows potentially indicating aneurysms (7.32%), conical narrowing (1.63%), focal bulging (1.63%), and wall irregularities (4.07%). Among 32 patients with arterial stenosis, the most frequent sites of stenosis were the posterior cerebral artery (PCA) and internal carotid artery (ICA), each observed in 12 patients (37.5%). This was followed by the anterior cerebral artery (ACA) in 9 patients (28.33%), middle cerebral artery (MCA) in 7 patients (21.88%), and vertebral artery (VA) in 5 patients (15.62%) (Table.1).HR-VWI in stenosis-confirmed cases demonstrated focal vessel wall thickening, contrast enhancement, and vasculitis-like features, suggesting possible immune-mediated endothelial injury (Fig.2). Further analysis revealed that stenosis severity was positively correlated with elevated antiphospholipid antibody titers, comorbid valvular heart disease, and cognitive impairment.
Conclusion: This study provides the first systematic evaluation of intracranial arterial stenosis in APS, revealing it to be a relatively common and potentially underrecognized manifestation. Multimodal imaging combining MRA, CTA, and HR-VWI offers a comprehensive strategy for early detection and characterization of CNS vascular involvement. These findings expand the vascular phenotype of APS and underscore the importance of early cerebrovascular surveillance in patients with high-risk clinical or serologic features.
.jpg) Table.1. Prevalence and Distribution of Intracranial Vascular Abnormalities in a Cohort of 123 Patients
Table.1. Prevalence and Distribution of Intracranial Vascular Abnormalities in a Cohort of 123 Patients
.jpg) Fig.2. High-Resolution Vessel Wall Imaging (HR-VWI) in a Patient with Intracranial Vascular Stenosis Associated with Antiphospholipid Syndrome (APS).
Fig.2. High-Resolution Vessel Wall Imaging (HR-VWI) in a Patient with Intracranial Vascular Stenosis Associated with Antiphospholipid Syndrome (APS).
To cite this abstract in AMA style:
Fan Y, Qian J, Wei X, Pan H, Yu S, Yang Z, Gu S, Wu J, Wang C, Zhou T, Shi H. Intracranial Arterial Stenosis in Antiphospholipid Syndrome: A Neglected Vascular Involvement? [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/intracranial-arterial-stenosis-in-antiphospholipid-syndrome-a-neglected-vascular-involvement/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/intracranial-arterial-stenosis-in-antiphospholipid-syndrome-a-neglected-vascular-involvement/