Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Antiphospholipid antibodies nephropathy (aPL-N) is defined by thrombotic microangiopathy (TMA) early lesions and late lesions such fibro-intimal hyperplasia with luminal obliteration/organized thrombi, fibrous arterial/arteriolar occlusion and focal cortical atrophy1.Beyon d these distinct microvascular lesions, other glomerular conditions (membranous nephropathy, MN; focal segmental glomerulosclerosis, FSGS), were reported in primary APS (PAPS) patients, even without aPL-related vascular lesions. Aim: 1) To evaluate clinical/laboratory features associated to intra-renal involvement in PAPS patients; 2) to clinically and histologically characterize PAPS patients with a) aPL-N and b) non-aPL-N intra-renal involvement.
Methods: Observational multicentric study including PAPS patients regularly followed (1984-2023). 1) Case-control study: PAPS patients with intra-renal involvement histologically confirmed vs PAPS patients without renal involvement signs. 2) Separate analysis according to renal histologic findings: a) aPL-N and b) non-aPL-N.
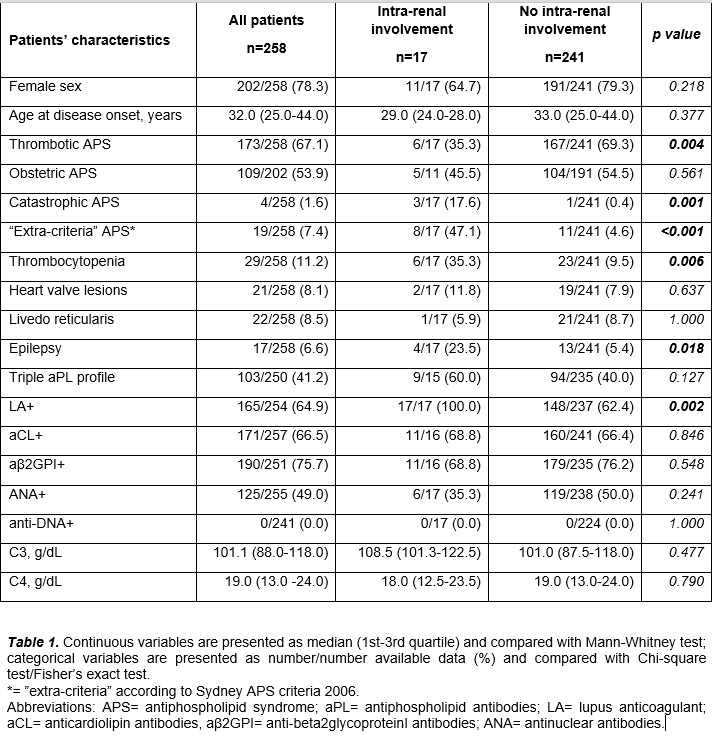
Results: Among 258 PAPS patients (78% females, median age at onset: 32 years, 67% thrombotic phenotype, 54% obstetric phenotype, 41% triple aPL+), 17 (7%) had histologically confirmed intra-renal involvement. It was the first disease manifestation in 10/17 (59%) patients, the main presentation was with isolated urinary abnormalities (IUAs) in 53% of the cases. At renal biopsy 35% had classic aPL-N injuries while 65% showed non-aPL-N intra-renal lesions. 1) Patients with intra-renal involvement suffered less macrovascular thrombotic events and more catastrophic APS (CAPS), thrombocytopenia, epilepsy, and lupus anticoagulant (LA)+ (Table 1). 2a) aPL-N was the first manifestation of APS in 5/6 (83%) cases, presenting with severe arterial hypertension in 17%, CAPS in 33% and IUAs in 50%. Despite therapy with anticoagulant (60%) or antiplatelet (40%) drugs in most patients, the 12-months renal response was complete in only 1/3 of the cases; half of the patients suffered subsequent aPL-related events (3/6 thrombocytopenia; 2/6 thrombotic events).
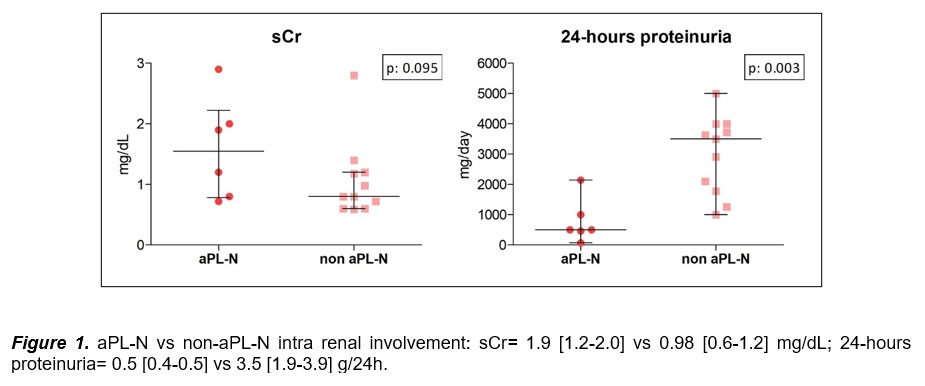
2b) PAPS patients with non-aPL-N intra-renal lesions had MN in 6/11 and FSGS in 5/11 cases, with some degree of non-specific vascular injury in 64%. As compared to patients with aPL-N, they presented more frequently normal serum creatinine and higher 24h-proteinuria levels (Figure 1) but no differences in systemic autoantibodies/complement levels. All the patients belonging to this subgroup experienced aPL-related events (8/11 thrombotic events, 5/6 obstetric events, 3/11 epilepsy, 2/11 heart valve lesions, 1/11 thrombocytopenia), that in 45% cases were preceded by the renal disease.
Conclusion: The present work highlights the importance of conducting appropriate renal study in PAPS patients with renal biopsy, if needed, even in presence of mild IUAs. It underscores that aPL-N, being part of the peculiar microvascular APS subset, may require a treatment strategy beyond anticoagulation2. From nephrologists’ perspective, routinary screening for aPL during the assessment of glomerulopathies could be relevant, given the aPL prognostic role in the development of subsequent related events.
To cite this abstract in AMA style:
Moschetti L, Sciascia S, Fredi M, Zappa M, Radin M, Cavazzana I, Affatato S, Nalli C, Andreoli L, Alberici F, Franceschini F, Roccatello D, Tincani A. Intra-renal Involvement in Primary Antiphospholipid Antibodies Syndrome: Data from Two Italian Centers [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/intra-renal-involvement-in-primary-antiphospholipid-antibodies-syndrome-data-from-two-italian-centers/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/intra-renal-involvement-in-primary-antiphospholipid-antibodies-syndrome-data-from-two-italian-centers/