Session Information
Session Type: Abstract Session
Session Time: 2:00PM-3:30PM
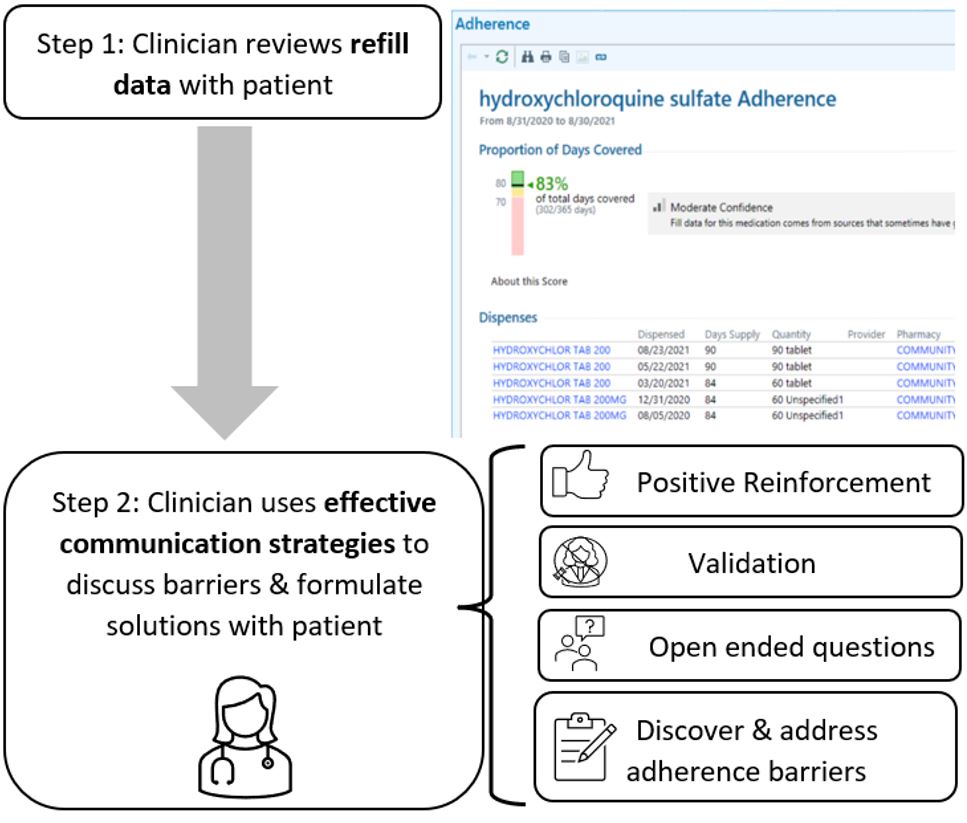
Background/Purpose: Medication nonadherence is common and is associated with increased disease activity, morbidity, and mortality in SLE. To optimize medication adherence and SLE outcomes, we developed a simple clinician-led adherence intervention that involves clinicians reviewing real-time pharmacy refill data during the encounter and using effective communication techniques with patients to collaboratively overcome adherence barriers (Figure 1). Prior pilot testing demonstrated intervention feasibility, acceptability, and preliminary effect on adherence. In this study, we aimed to examine how the intervention is performed in practice and identify areas for improvement to inform future implementation.
Methods: We audio recorded clinic encounters between clinicians and patients seen at an academic lupus clinic. Patients were included if they had 90-day medication possession ratio (MPR) < 80% for SLE-specific medications. We coded which intervention components clinicians performed, quality of patient-clinician communication, and time spent discussing adherence. Following the intervention encounter, we also conducted audio-recorded semi-structured interviews with patients and clinicians about their experiences with the intervention and analyzed the data using applied thematic analysis. Lastly, we assessed change in 90-day MPR after the intervention visit and considered a 20% increase as major improvement.
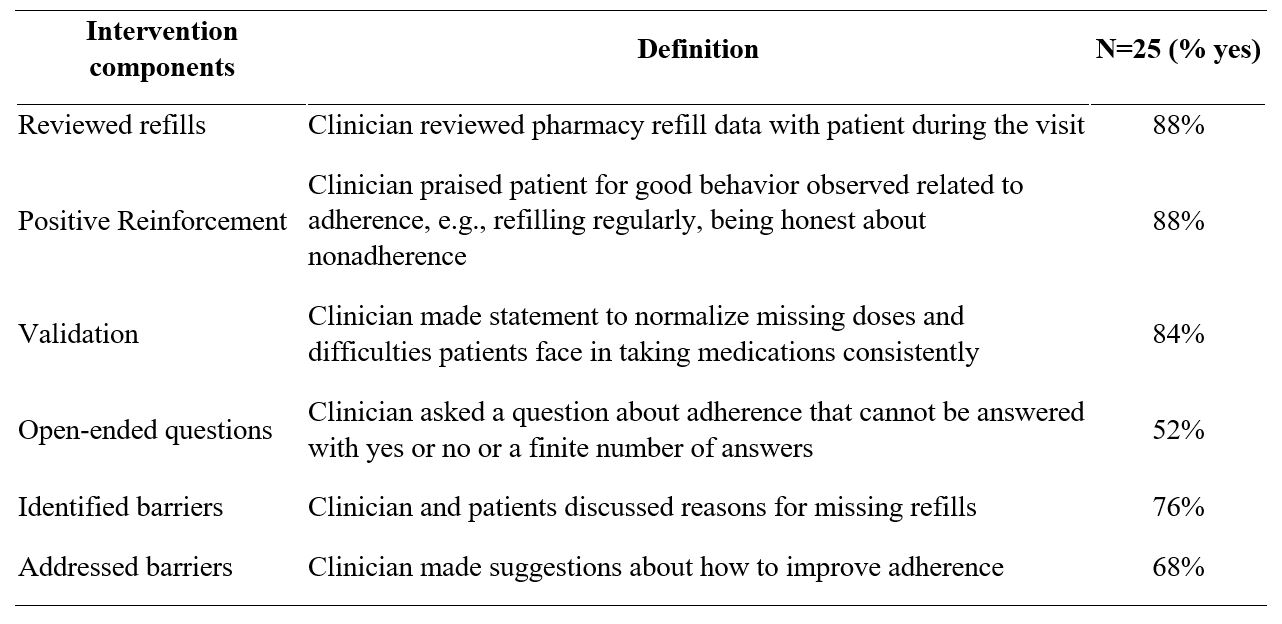
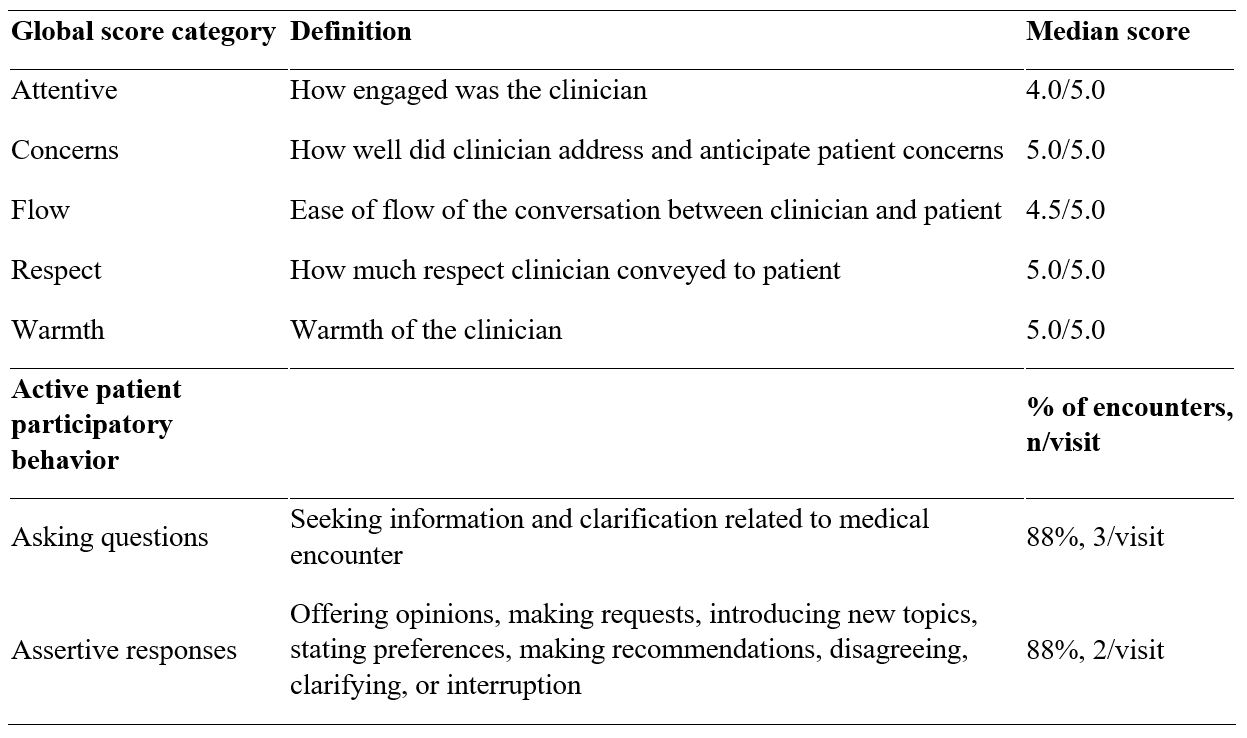
Results: We recorded and analyzed 25 patient encounters (median age 39, 100% female, 72% Black) among 6 clinicians. Clinicians performed the majority of intervention components in most of encounters, suggesting fidelity (Table 1). Global communication scores and rates of active patient participation were high, suggesting excellent communication. Adherence discussions took on average 3.8 minutes.
Nineteen patients and 5 clinicians completed in-depth interviews. Nearly all participants felt the time spent discussing adherence was just right and necessary. Almost all patients felt the intervention was useful. Many patients described feeling heard and valued, being more honest about nonadherence, and being more knowledgeable and motivated to take SLE medications. Clinicians described less judgmental adherence discussions as a result of the intervention. To improve the intervention, patients emphasized better patient-clinician communication and wanted help problem solving financial and logistical barriers. Clinicians suggested additional resources and training to improve adherence conversations and utilizing peer support and other staff in the intervention.
Following the intervention visit, almost half (48%) of patients had a major improvement ( >20% increase) in MPR.
Conclusion: Our findings suggest that this intervention can be performed with high fidelity in a short amount of time. It encouraged high quality communication and improved adherence. Both patients and clinicians described positive experiences with the intervention. Future work will focus on optimizing clinician training, exploring ways to increase the intervention’s efficiency and effectiveness, and testing the intervention in a larger controlled setting.
To cite this abstract in AMA style:
Sun K, Molokwu N, Hanlen E, Corneli A, Pollak K, Rogers J, Sadun R, Criscione-Schreiber L, Doss J, Bosworth H, Clowse M. Intervention to Improve Medication Adherence Among Patients with SLE [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/intervention-to-improve-medication-adherence-among-patients-with-sle/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/intervention-to-improve-medication-adherence-among-patients-with-sle/