Session Information
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: In rheumatoid cachexia (RC), high resting energy expenditure (REE) has been associated with loss of muscle mass driven by proinflammatory cytokines. The objectives of this study were to evaluate alterations of REE, body composition, metabolic parameters and physical function in individuals with RA, and to investigate the interaction between systemic inflammation and modifiable risk factors for RC on REE.
Methods: A prospective, cross-sectional study was performed in RA individuals (n=35) and age/sex/race/BMI-matched healthy controls (n=11). Participants underwent measures for REE by indirect calorimetry, body composition by dual energy x-ray absorptiometry, in addition to anthropometric, biochemical and DAS-28 CRP measures. Physical activity (METs, total activity count/ day and step counts) and physical performance (5-repetition sit-to-stand, knee extensor MVIC and 5-repetition average power) data were also collected. Dietary intakes were estimated using consecutive four-day food records. Homeostasis model assessment for insulin resistance (HOMA-IR) and serum interleukin-6 (IL-6) were used as parameters of insulin resistance (IR) and systemic inflammation, respectively. Regression models tested association between REE and dependent variables, including pre-specified interaction tests involving HOMA-IR and IL-6 and dietary protein intake and IL-6.
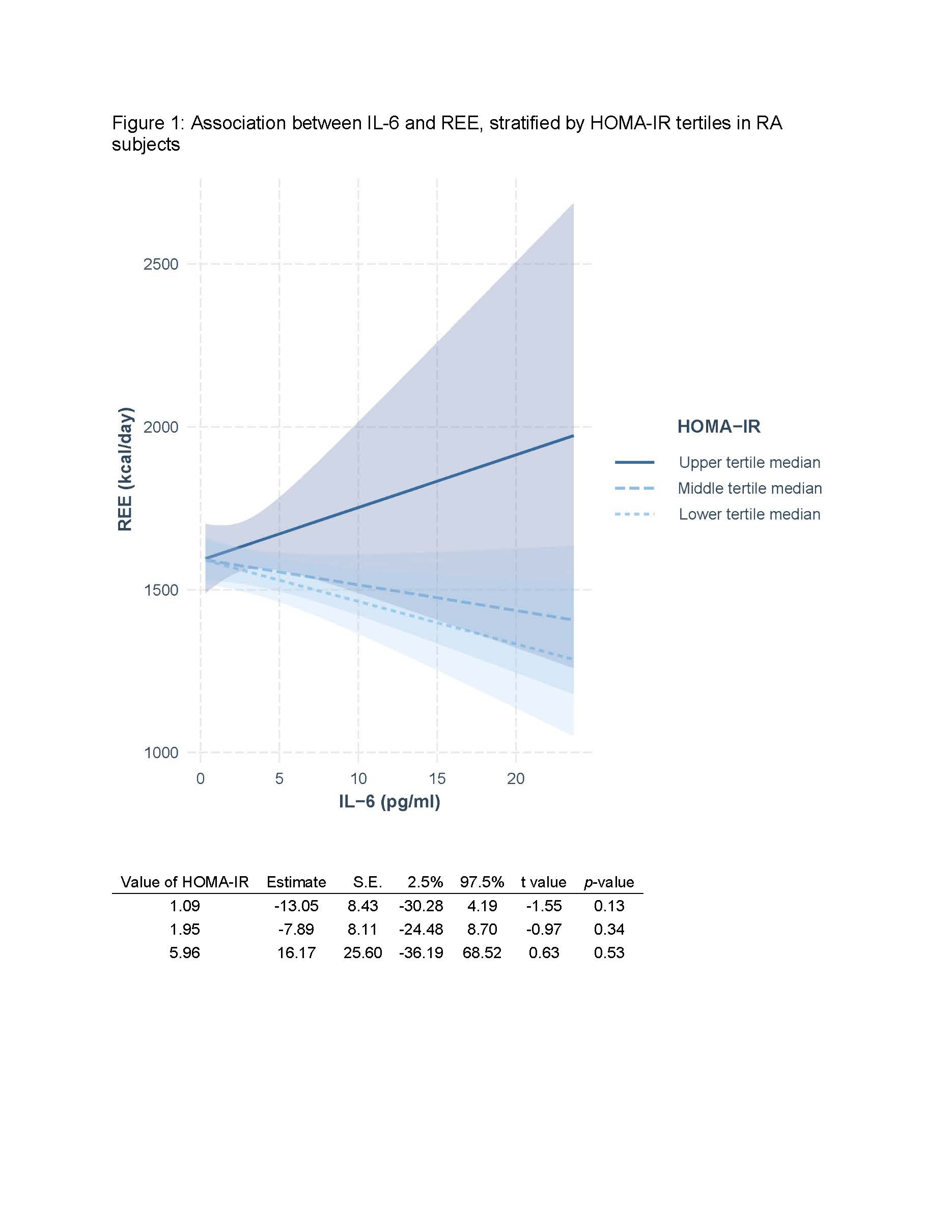
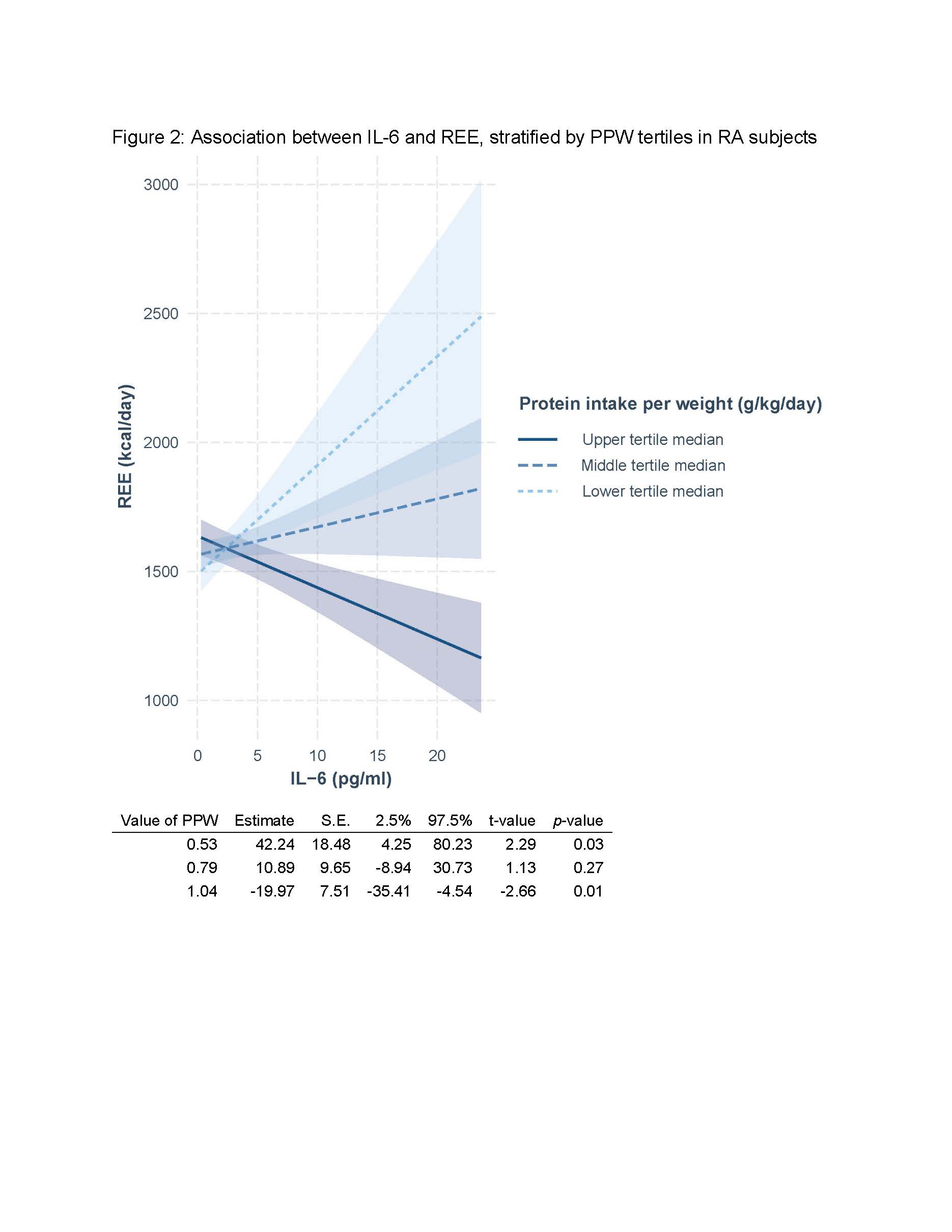
Results: RA subjects were mostly women (94%), with a median age of 54 years (50.5, 70), BMI of 30.5 kg/m2 (26.1, 36.9), disease duration of 7.8 years (4.9, 18.1) and DAS-28 CRP of 1.77 (1.2; 2.8). Approximately two-thirds of RA subjects were either positive for rheumatoid factor on anti-CCP. Only 17% of RA subjects were on prednisone, at a median dose of 5.0 mg/ day (4.0, 5.0), and all RA subjects were on DMARD therapy. RA subjects demonstrated significantly lower levels of physical activity [METs (p= 0.004), total activity count/ day (p=0.03), step counts (p=0.001)], poorer physical performance [5-repetition sit-to-stand (p=0.002), knee extensor maximum voluntary isometric contraction (MVIC, p=0.03) and higher levels HOMA-IR (p=0.006)] compared to non-RA controls. Fat mass index [FMI] (p=0.06) and fat free mass index [FFMI] (p= 0.33) were not significantly different between RA and non-RA controls. Among RA subjects, HOMA-IR (β= 4.66; p=0.80), IL-6 (β=-9.45; p=0.24) and the interaction between HOMA-IR and IL-6 (β= 6.00; p=0.29) were not significantly associated with REE, after adjustment for age and FFMI. However, we observed a significant interaction effect between protein intake per weight (PPW) and serum IL-6 on REE among RA subjects in the multivariate model. The upper tertile of PPW demonstrated a significant negative correlation between REE and IL-6 (β=-19.97, 95% CI [-35.41, -4.54], p=0.01). The lower tertile of PPW demonstrated a significant positive correlation between REE and IL-6 (β=42.24, 95% CI [4.25, 80.23], p=0.03).
Conclusion: Inflammation is likely a common antecedent leading to both elevated REE and IR in patients with RA. While IR can lead to muscle catabolism, IR does not seem to be a major driver of REE in patients with RA. Higher dietary protein intake could attenuate the effect of systemic inflammation on REE in RA patients.
To cite this abstract in AMA style:
Hanaoka B, Zhao J, Heitman K, Khan F, Brock G, Volek J, Jarjour W, Gower B. Interaction Effect of Systemic Inflammation and Dietary Protein Intake on Resting Energy Expenditure in Individuals with RA [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/interaction-effect-of-systemic-inflammation-and-dietary-protein-intake-on-resting-energy-expenditure-in-individuals-with-ra/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/interaction-effect-of-systemic-inflammation-and-dietary-protein-intake-on-resting-energy-expenditure-in-individuals-with-ra/