Session Information
Date: Sunday, November 12, 2023
Title: (0543–0581) SLE – Diagnosis, Manifestations, & Outcomes Poster I
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Systemic lupus erythematosus (SLE) patients more commonly have insulin resistance (IR) than control subjects. Recent studies have revealed that the complement (C) system is not only a mediator of the immune system but is also related to the pathogenesis of atherosclerosis in the general population. Given that the C alteration is a characteristic of SLE, in the present work we set out to analyze if there is a relationship between the C system and IR in patients with SLE.
Methods: New generation functional assays of the three pathways of the C system were performed in 225 non-diabetic patients with SLE. In addition, the serum levels of inactive (C1q, C2, C3, C4, factor D), activated (C3a) and regulators (C1 inhibitor and factor H) molecules of the C system were evaluated. Insulin and C-peptide serum levels were measured, and insulin resistance and indices of beta cell function were calculated using the homeostatic model assessment –HOMA–. Metabolic syndrome criteria fulfillments were applied. Multivariable linear regression analysis was performed to assess the relationship between C system and IR indices and the presence of metabolic syndrome.
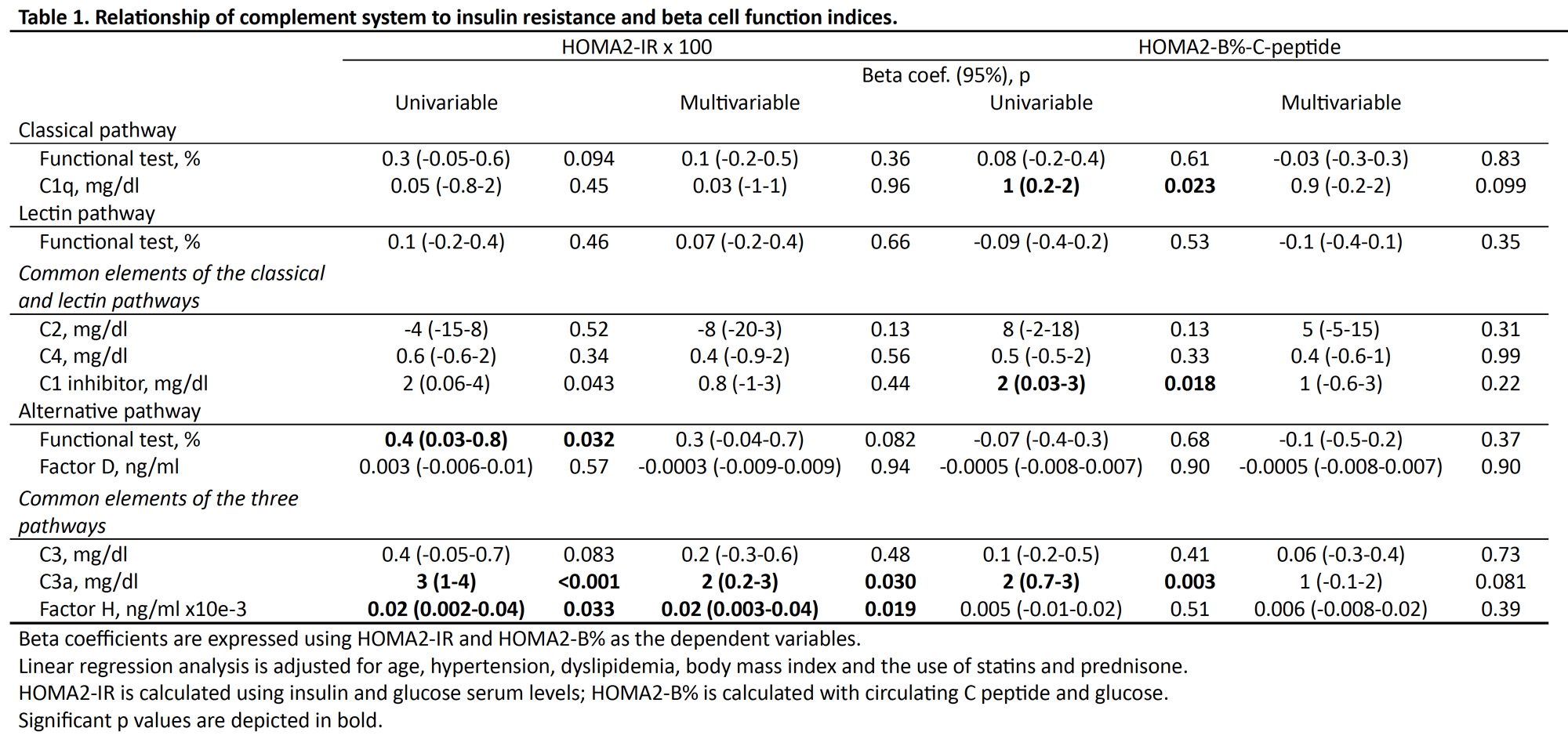
Results: C system pathways functional tests and individual elements showed significant relationships with IR indices in the univariable and multivariable analysis (Table 1). In this regard, after multivariable analysis that included age, hypertension, dyslipidemia, BMI and the use of statins and prednisone, serum C3a and factor H values were associated with higher HOMA2-IR levels. In contrast, after adjusting for covariates, no relationship was found between system C and the HOMA2-B% index expressing β-cell function.
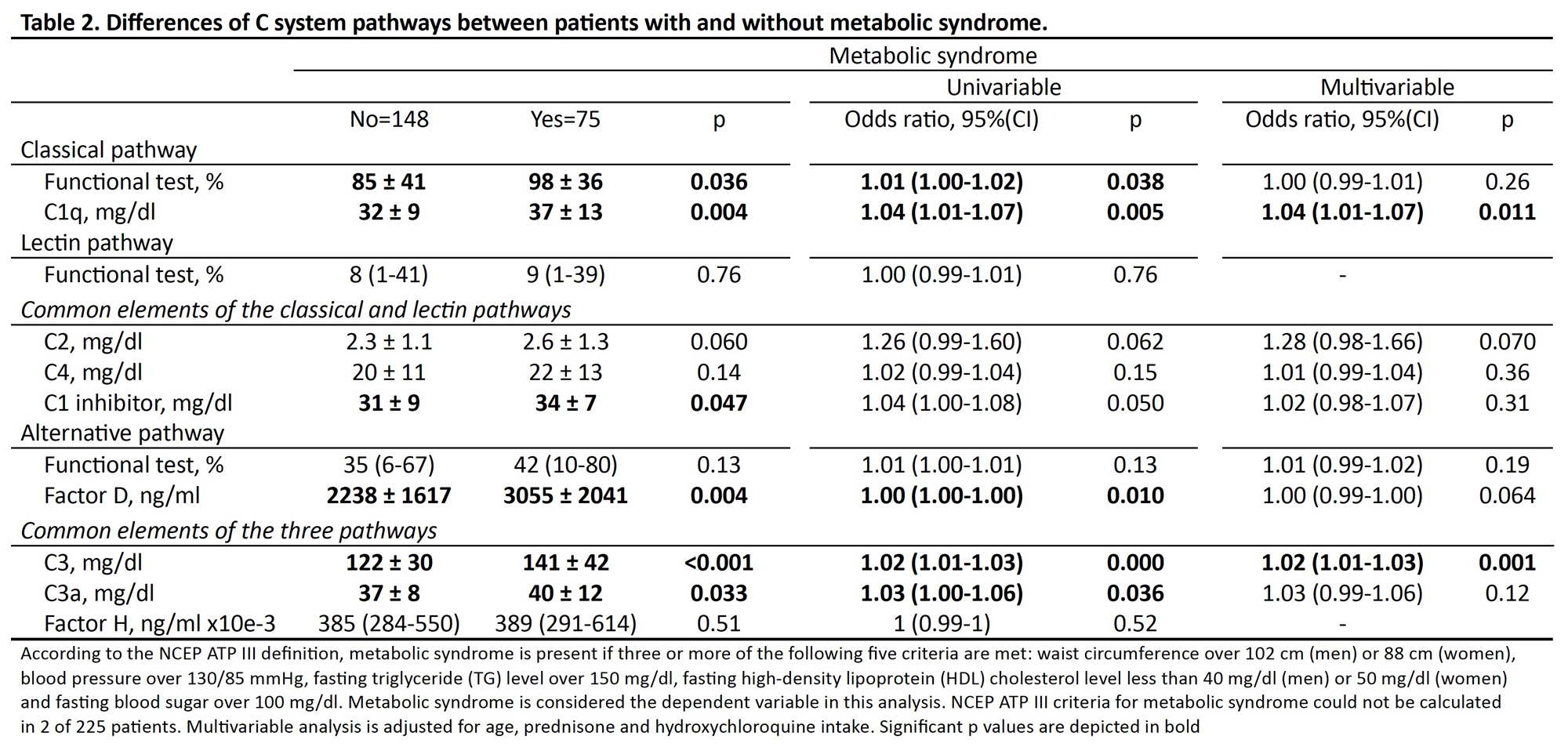
Seventy-five (33%) patients fulfilled the definition of metabolic syndrome using the NCEP ATP III criteria. As expected, patients with metabolic syndrome were significantly older, used statins and antihypertensive treatment more frequently, suffered more commonly obesity and dyslipidemia, and had higher values of BMI and abdominal circumference. Regarding disease-related data, in the univariable analysis, patients with metabolic syndrome had more accrual damage measured through the SDI score, and less frequently were taking hydroxychloroquine when the study was performed.
Besides, SLE patients with metabolic syndrome had some differences in C system routes functional assays and inactive and active individual C elements. With respect to this, in the univariable analysis, patients with metabolic syndrome exhibited higher serum levels of C1q, factor D, C3, C3a and C1-inh (Table 2). Besides, in the multivariable analysis, after adjustment for covariates, serum levels of C1q and C3 were associated with a higher odds ratio for the presence of metabolic syndrome (Table 2).
Conclusion: IR and metabolic syndrome are positively and independently related to higher serum levels of some serum C elements in patients with SLE with a predominant role of the alternative pathway elements.
To cite this abstract in AMA style:
Viotti-Serra J, García-González M, Gómez-Bernal F, Quevedo-Abeledo J, Fernández-Cladera Y, González-Rivero A, Gonzalez-Gay M, Ferraz Amaro I. Insulin Resistance and the Complement System Are Linked in Patients with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/insulin-resistance-and-the-complement-system-are-linked-in-patients-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/insulin-resistance-and-the-complement-system-are-linked-in-patients-with-systemic-lupus-erythematosus/