Session Information
Date: Sunday, November 5, 2017
Title: Spondyloarthropathies and Psoriatic Arthritis – Clinical Aspects and Treatment Poster I
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: The effect of local inflammation on structural damage in patients (pts) with axial spondyloarthritis is not well known. We aimed to test the possible effect of inflammation on structural damage both assessed by MRI and at the level of the spine and SIJ.
Methods: Pts with recent onset (≤3 years) axSpA (according to the treating rheumatologist) from the DESIR cohort were included. MRI of the SIJ (MRI-SIJ) and spine (MRI-spine) were obtained at baseline (BL), 2 and 5 years and scored by 3 trained central readers. Bone Marrow Edema (BME) at MRI-SIJ was assessed according to ASAS definition and at the MRI-spine by the presence of ≥ 3 lesions. Structural damage in the SIJ (MRI-SIJ-STR) and in the spine (MRI-spine-STR) was defined by ≥ 3 fatty lesions. The % of structural net progression (number of ‘progressors’ minus the number of ‘regressors’ divided by total number of pts) was assessed according to CRP and BME status at BL. The effect of BME on MRI-SIJ on MRI-SIJ-STR and of BME on MRI-spine on MRI-spine-STR was evaluated using two types of binomial generalized estimating equations (GEE) models: i. effect at BL on 5 years incorporating measurements from all readers (GEE adjusted for reader); ii. effect of BME over 5 years (longitudinal time-lagged models with auto-regression). The final models were adjusted for variables proved to confound the association of interest (variables tested: age, gender, HLA-B27, smoking status, CRP, BASDAI, ASDAS, treatment with NSAIDs and TNFi).
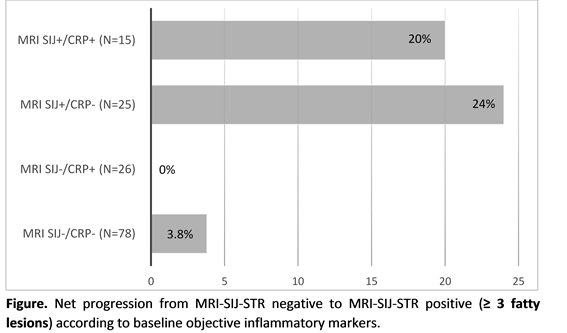
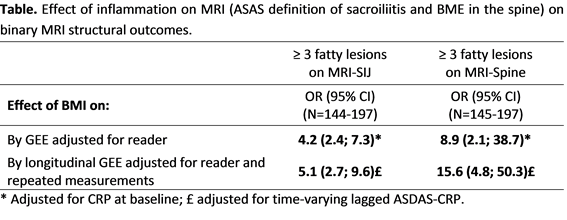
Results: In total, 151 and 145 pts had complete 5-year MRI-SIJ and MRI-spine data available from 3 readers, respectively. Of the 151 pts with complete MRI-SIJ data, the net % pts who switched from MRI-SIJ-STR negative to positive ranged from 3.8% to 24% according to the presence of objective signs of inflammation at BL (figure). Low number of pts did not allow for similar analysis in the spine. In the multivariable analysis, both the presence of BME at MRI-SIJ (OR=4.2 [95% CI: 2.4-7.3]), and BME at MRI-spine (OR=8.9 [95% CI: 2.1-38.7]) at baseline were highly predictive of MRI-SIJ and MRI-spine structural progression respectively 5 years later, adjusting for CRP (only factor found to confound the association of interest). Similar positive associations were found in the longitudinal models testing the effect of BME on MRI-SIJ-STR and MRI-spine-STR over 5 years (table).
Conclusion: Our results show that local inflammation is strongly associated with the development of structural damage over 5 years both in the SIJ and spine in early axSpA and that this effect is independent of systemic inflammation.
To cite this abstract in AMA style:
Sepriano A, Ramiro S, Landewé RBM, Dougados M, van der Heijde D. Inflammation on MRI of Spine and Sacroiliac Joints Is Highly Predictive of Structural Damage in Axial Spondyloarthritis: The 5 Years Data of the DESIR Cohort [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/inflammation-on-mri-of-spine-and-sacroiliac-joints-is-highly-predictive-of-structural-damage-in-axial-spondyloarthritis-the-5-years-data-of-the-desir-cohort/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/inflammation-on-mri-of-spine-and-sacroiliac-joints-is-highly-predictive-of-structural-damage-in-axial-spondyloarthritis-the-5-years-data-of-the-desir-cohort/