Session Information
Date: Saturday, November 6, 2021
Title: Health Services Research Poster I: Lupus, Inflammatory Arthritis, & More (0128–0148)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: The association between systemic lupus erythematosus (SLE) and cardiovascular disease has been well-studied. Cardiovascular disease is a risk factor for major adverse cardiac events (MACE) after surgery. The objective of this study was to estimate the risk of MACE in patients with SLE undergoing moderate to high-risk non-cardiac surgeries compared to control patients with and without diabetes.
Methods: This retrospective, observational study used deidentified administrative data from the Optum Clinformatics Data Mart to identify adult patients who underwent non-cardiac surgery in 2007-2020 via Current Procedural Terminology (CPT) codes. Two independent providers (SB, BB) omitted low risk procedures such as simple skin procedures, endoscopies, ocular surgeries, or orthopedic surgeries that were distal to the elbow or knee joints. From this pool, we defined a SLE cohort (patients who had two or more international classification of diseases (ICD) 9 or 10 codes of 710.0 or M32.xx but not M32.0 within one year before surgery), a diabetic cohort, and a non-diabetic cohort. We matched SLE cases with the diabetic and non-diabetic cohorts by age and gender. Our primary outcome was MACE (including death, myocardial infarction, ischemic stroke, or pulmonary embolism defined by ICD or CPT codes) within one month post-surgery. We performed a multivariable conditional logistic regression to estimate the odds of MACE within one month of surgery for the three cohorts after adjusting for pre-operative Revised Cardiac Risk Index (RCRI) scores and race (white, black, Hispanic, Asian, and unknown). The RCRI scores include congestive heart failure, coronary artery disease, insulin-dependent diabetes, cerebrovascular disease, and chronic kidney disease (all these variables were defined by claims). Scores greater than one are considered moderate to high risk. We also performed multivariable logistic regression models for MACE amongst SLE patients only that included RCRI scores, age, gender, race, and SLE disease activity (Garris index).
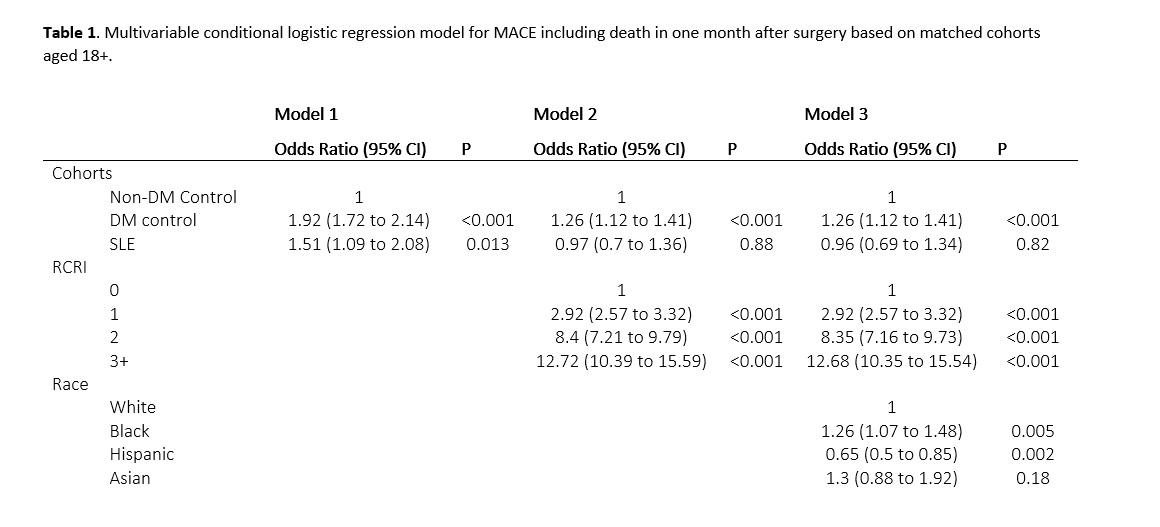
Results: We included 4,750 SLE patients, 484,986 non-diabetes controls, 496,381 diabetes controls and After matching, no significant differences were observed between SLE and diabetic patients in MACE rates. Without adjustment, SLE patients had an increased risk of MACE compared to non-diabetic controls (Table 1, OR 1.51, 95% CI 1.09-2.08); however, the association became nonsignificant after adjusting for RCRI scores (OR 0.97, 95% CI 0.70 – 1.36. Amongst SLE patients, higher RCRI scores, older age, and non-white race were associated with increased risks of MACE, but not gender, pre-operative cardiac testing, or SLE disease activity.
Conclusion: Patients with SLE have an increased risk of MACE within one month after surgery similar to diabetes controls but higher than non-diabetes controls. This risk normalizes after adjusting for pre-operative RCRI scores, suggesting that SLE patients are at an increased risk of MACE because of underlying comorbidities including cardiovascular disease. Our results indicate that SLE confers an increased risk for MACE, independently of disease severity, mediated by pre-existing cardiovascular disease.
To cite this abstract in AMA style:
Bruera S, Lei X, Blau B, Zhao H, Deswal A, Yazdany J, Giordano S, Suarez-Almazor M. Increased Risk of Major Adverse Cardiac Events in Patients with Systemic Lupus Erythematosus After Non-Cardiac Surgery [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/increased-risk-of-major-adverse-cardiac-events-in-patients-with-systemic-lupus-erythematosus-after-non-cardiac-surgery/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/increased-risk-of-major-adverse-cardiac-events-in-patients-with-systemic-lupus-erythematosus-after-non-cardiac-surgery/