Session Information
Date: Sunday, November 12, 2023
Title: (0176–0195) Healthcare Disparities in Rheumatology Poster I: Lupus
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Systemic Lupus Erythematosus (SLE) is more prevalent and has greater adverse health outcomes in women, minorities, and individuals with low socioeconomic status (SES), particularly in Medicaid populations. These associations have not been reported in the Medicare population of older or disabled individuals. Our purpose is to analyze the association between environments of social vulnerability and SLE prevalence and acute hospital events in a Medicare population within the United States.
Methods: This was a cross-sectional study utilizing the Centers for Disease Control and Prevention (CDC)/Agency for Toxic Substances and Disease Registry (ATSDR) Social Vulnerability Index (SVI) and Lupus Research Alliance Lupus Index Medicare data at a county level. Individuals enrolled in fee-for-service Medicare in 2016 who were diagnosed with SLE by 2 or more ICD-9 codes 30 or more days apart were included. We examined the association between the prevalence of and acute hospital event rates among SLE patients and overall, SVI rank, 4 themes, and 15 subthemes within each county.
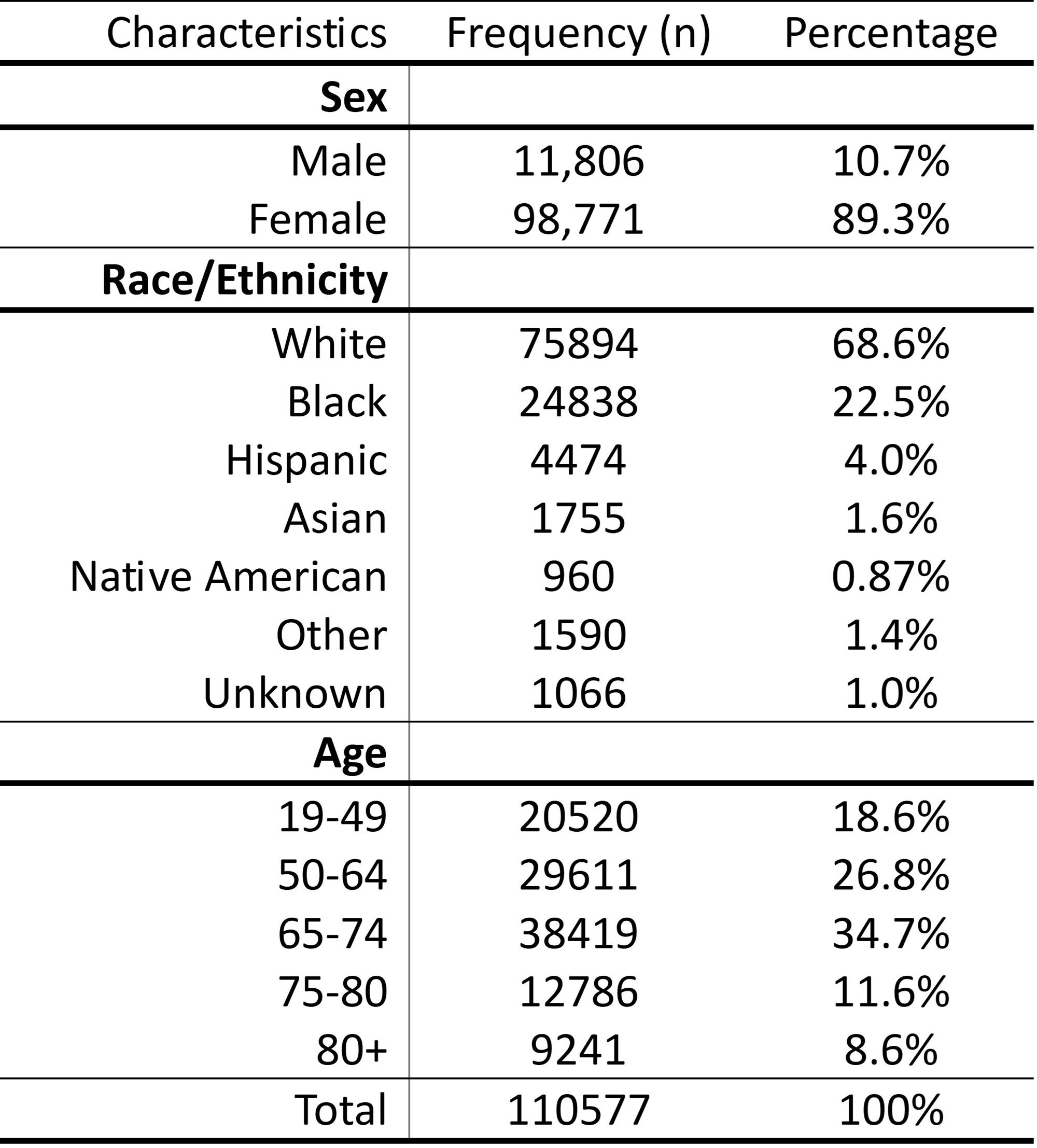
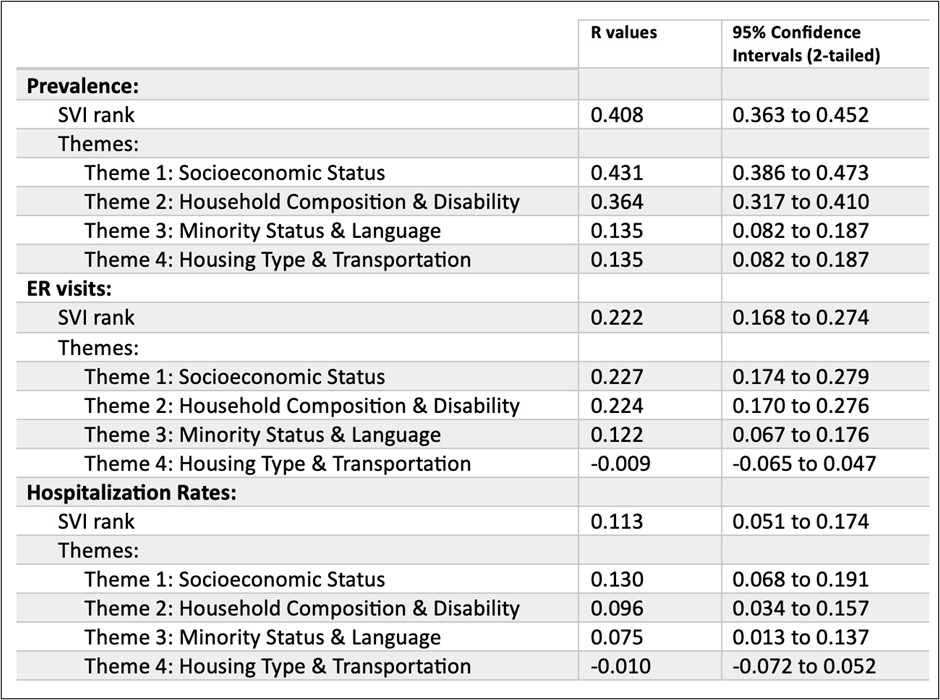
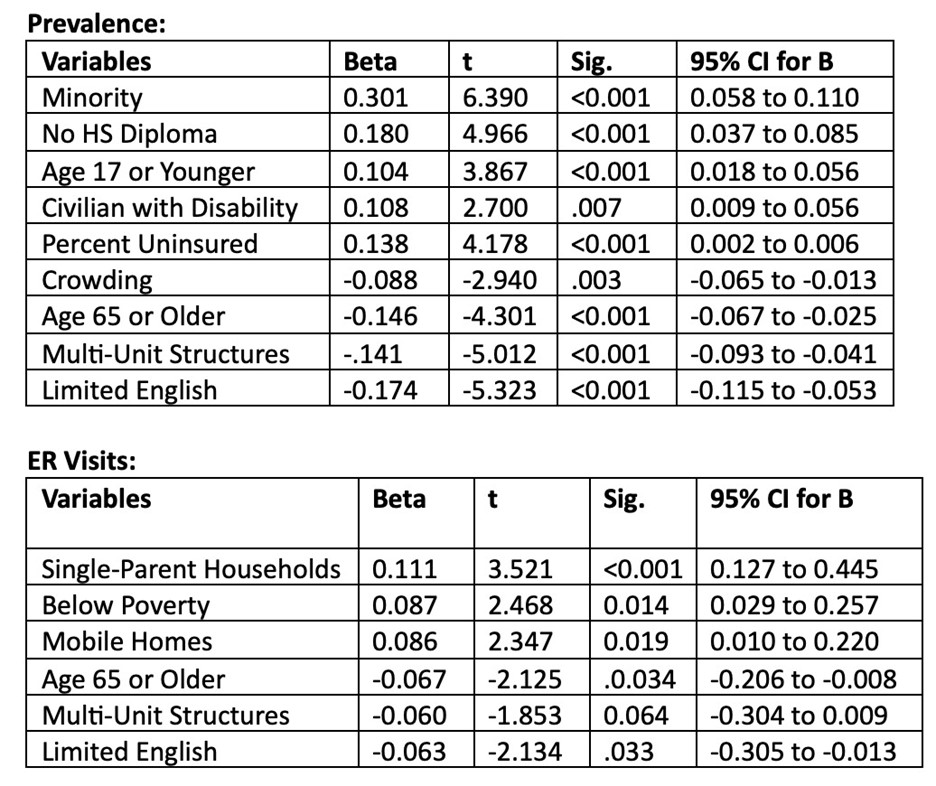
Results: The Medicare SLE population was primarily composed of female and White patients (Table I). Using ranked correlation, SVI themes and each of subthemes 1-4 were positively correlated with SLE prevalence, especially themes 1 and 2 (SES and Household Composition and Disability) (Table II). Themes 1 and 2 were positively correlated with ER visits, while theme 4 (Household type and Transportation) was negatively associated with ER visits (Table II). SVI themes and hospitalization rates were the least strongly correlated, however themes 1,2 and 3 (Minority and Non-English-speaking) were positively correlated, while theme 4 was negatively correlated (Table II). In backward stepwise logistic regression analysis, several subthemes were important in the models of prevalence and ER visit rates (Table III). SLE Prevalence was the variable most strongly correlated with SVI themes.
Conclusion: These findings mirror those from studies of SLE prevalence and ED visits in Medicaid populations as well as COVID prevalence and heat-exposure ED visits in socially vulnerable non-SLE patients. This suggests that environments of social vulnerability are an independent risk factor, but the elements of the environments (social stress, toxins, infrastructure, and proximity to care providers) that may drive risk are not addressed by this study. To our knowledge, no other study has examined SLE prevalence and acute hospital events within the Medicare population. These findings inspire the hypothesis that risk models can be used as a tool to identify at risk populations for strategic intervention to reduce disparities in outcomes.
To cite this abstract in AMA style:
Cosentino E, Pearce J, Oates J. Increased Prevalence of and Acute Hospital Events Among Medicare Systemic Lupus Erythematosus Patients Living in Socially Vulnerable Counties in the United States [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/increased-prevalence-of-and-acute-hospital-events-among-medicare-systemic-lupus-erythematosus-patients-living-in-socially-vulnerable-counties-in-the-united-states/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/increased-prevalence-of-and-acute-hospital-events-among-medicare-systemic-lupus-erythematosus-patients-living-in-socially-vulnerable-counties-in-the-united-states/