Session Information
Date: Monday, November 18, 2024
Title: Osteoporosis & Metabolic Bone Disease – Basic & Clinical Science Poster
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
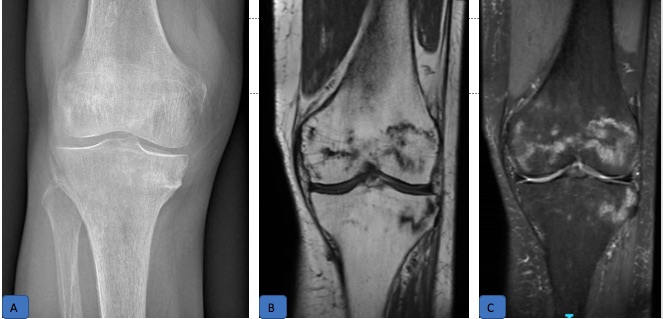
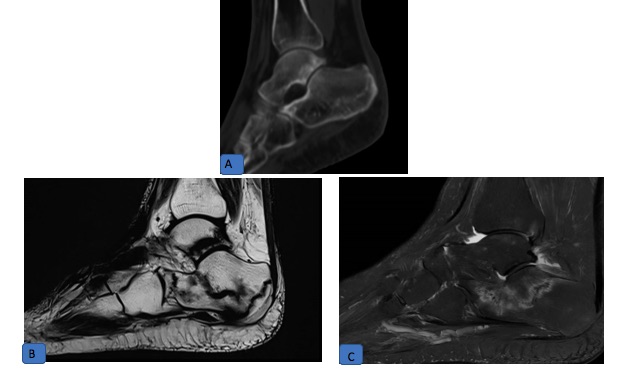
Background/Purpose: Spontaneous lower limb insufficiency fractures (LLIF) described under prolonged exposure to low-dose methotrexate are often bilateral, multiple, and recurrent. They share a common pathognomonic feature of a longitudinal band-like fracture along the growth plate of the bones in the lower limbs.
Methods: We conducted a retrospective case note review of patients who experienced MTX insufficiency fractures. Collected data included patient demographics, clinical and radiological features of the fractures, and bone health assessment results, including DXA scans. For patients with a typical MTX insufficiency fracture, we documented all subsequent fractures and whether MTX treatment was continued after the initial insufficiency fracture. The impact of continuing MTX on the timing and incidence of subsequent fractures was analyzed using Kaplan–Meier analysis.
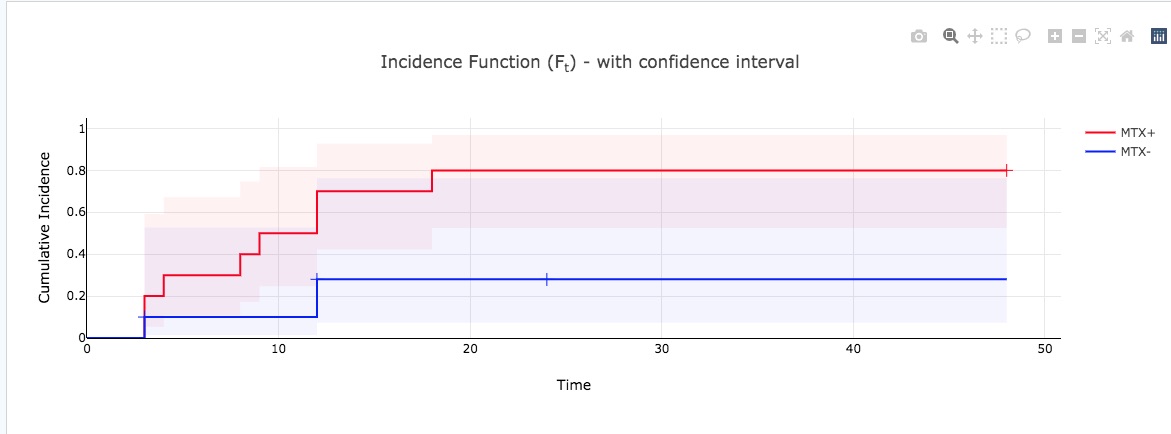
Results: We identified 10 patients with characteristic Methotrexate lower limb insufficiency fractures (MTX LLIF). The mean age at the presentation of the first fracture was 70 ± 12 years, with most patients (90%) being women and having rheumatoid arthritis (80%). At the time of the first LLIF, the mean MTX dose was 21 ± 5.2 mg weekly, with a cumulative dose of 7.5 ± 5 g. A predominance of subcutaneous administration (80%) was observed, with an average treatment duration of 7.7 ± 5.2 years. Only 4 patients received glucocorticoids at the time of the first LLIF, with a cumulative dose of 0.9 g ± 0.2 over the last year. The fracture sites were consistent with previous reports, with the metaphysis of the distal tibia (60%) and calcaneus (100%) being most commonly affected. Typical radiographic features of MTX LLIF are shown in Figures 1 & 2. One-third (30%) of patients had osteoporosis as assessed by DEXA, with a mean spine T-score of -0.7 ± 0.1 and a femoral neck T-score of -2.2 ± 0.6. Additionally, 30% were treated for osteoporosis prior to the first MTX insufficiency fractures, and the majority (7/10) were started on or continued osteoporosis treatment after the first insufficiency fracture.All patients continued MTX after the first LLIF for a mean duration of 23 ± 11 months due to diagnostic delay. After the first LLIF, 90% of patients sustained further LLIF with a mean number of recurrent fractures of 5.8 ± 4.5 and a mean interval of 9.8 ± 4.7 months between recurrent fractures. Upon diagnosis of MTX LLIF, all patients stopped MTX. Clinical improvement was apparent at 3 months (VAS pain, walking distance). A Kaplan-Meier analysis (Figure 3) showed the significant difference on fracture rates over time before and after stopping Methotrexate (Log Rank test, p=0.08)
Conclusion: Early diagnosis of Methotrexate lower limb insufficiency fractures (MTX LLIF) and prompt discontinuation of methotrexate are crucial to prevent recurrent fractures. Our study highlights the high risk of further fractures in patients who continue methotrexate treatment after the initial fracture. Stopping methotrexate significantly reduces the incidence of recurrent fractures, emphasizing the need for timely intervention and careful management in patients on long-term methotrexate therapy.
To cite this abstract in AMA style:
Ghossan R, FOGEL O, Roux C, Briot K. Increased Fracture Rates in Patients Continuing Methotrexate After Methotrexate-associated Lower Limb Insufficiency Fractures: A Retrospective Follow-up Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/increased-fracture-rates-in-patients-continuing-methotrexate-after-methotrexate-associated-lower-limb-insufficiency-fractures-a-retrospective-follow-up-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/increased-fracture-rates-in-patients-continuing-methotrexate-after-methotrexate-associated-lower-limb-insufficiency-fractures-a-retrospective-follow-up-study/