Session Information
Date: Saturday, November 16, 2024
Title: Abstracts: Miscellaneous Rheumatic & Inflammatory Diseases I
Session Type: Abstract Session
Session Time: 3:00PM-4:30PM
Background/Purpose: Patients with polymyalgia rheumatica (PMR) may develop overt giant cell arteritis (GCA), but “subclinical” large vessel inflammation has also been reported in patients with PMR. Whether or not this results in an elevated risk of aortic complications is unclear. Our objective was to describe the risk of aortic complications among patients with PMR as compared to those with GCA and a general population control group.
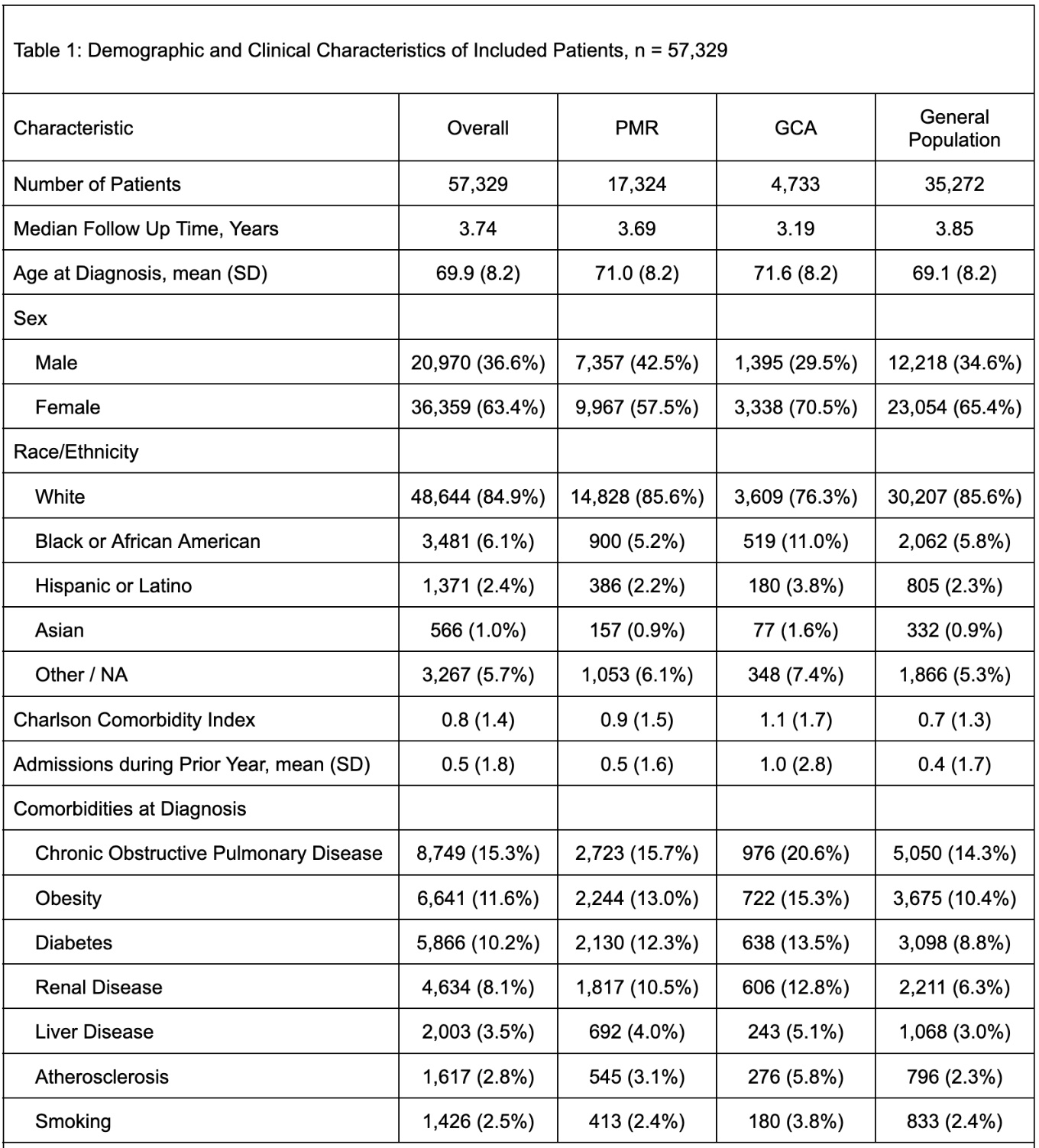
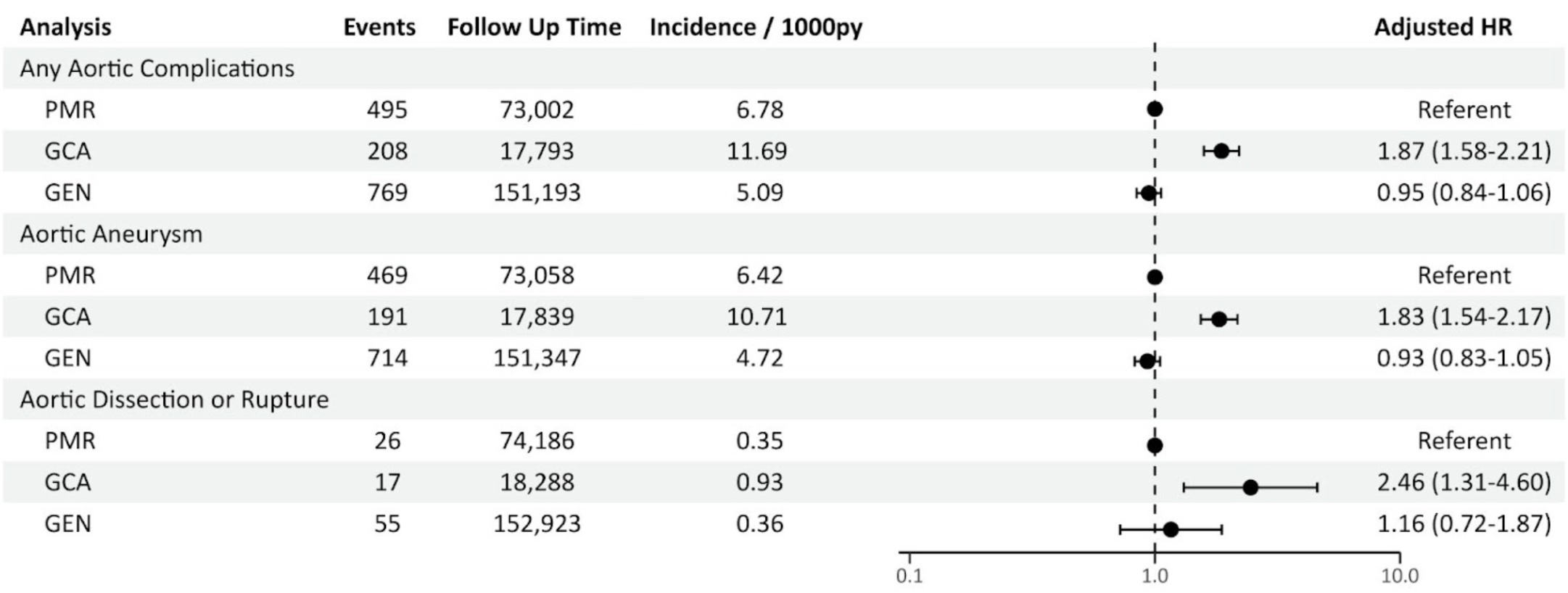
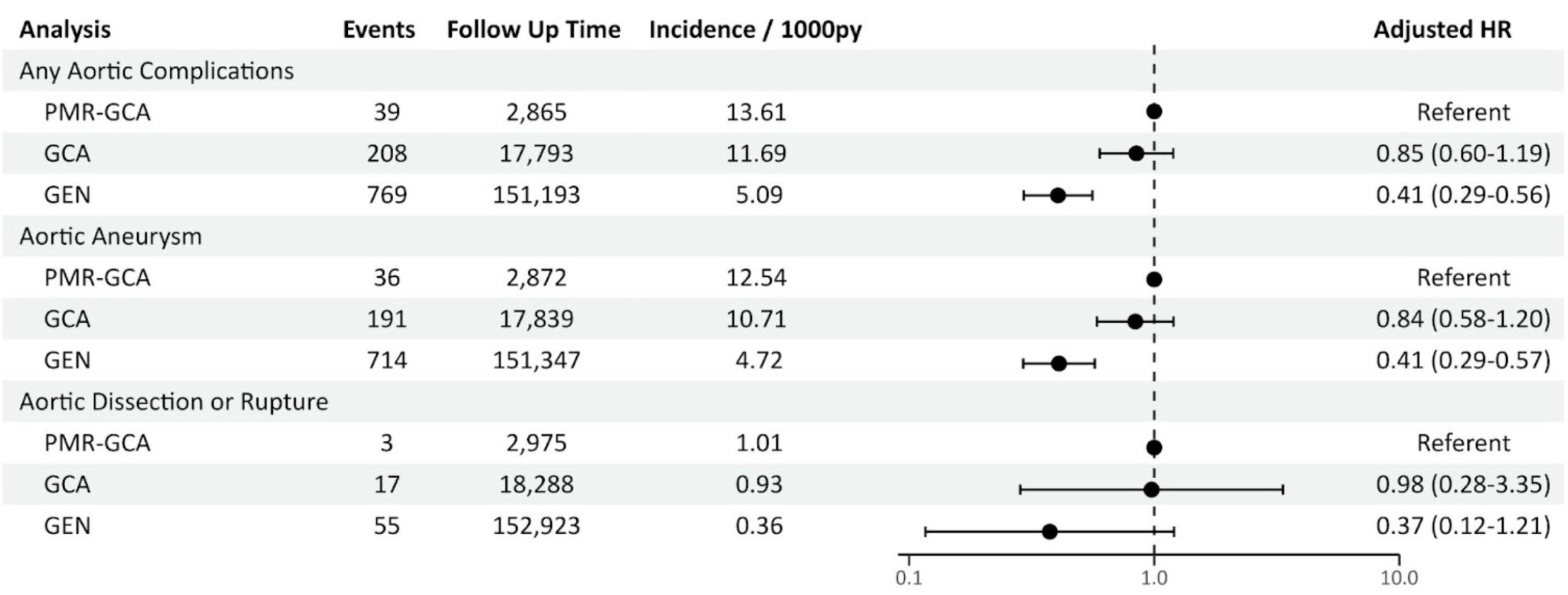
Methods: Using the US-based TriNetX electronic health records database (2000-2024), patients with ≥2 ICD-9/ICD-10-CM diagnostic codes for PMR or GCA between ≥30 days and < 365 days were included. The index date was the first prescription of corticosteroid and was required to occur within 30 days of the first PMR/GCA code. The PMR cohort was also matched to general population controls in 1:3 ratio. Patients were matched by sex, race/ethnicity, regional location, birth year, year of cohort entry, and year of cohort exit. The primary outcome was a composite of aortic aneurysm and aortic dissection or rupture. Unadjusted incidence rates were reported and adjusted hazard ratios (aHR) were calculated using Cox proportional cause-specific hazard models with PMR as the referent category. A sensitivity analysis of patients who had PMR but later developed GCA (PMR-GCA), which set the onset of GCA as the index date, was also performed.
Results: A total of 57,329 were identified, including 17,324 patients with PMR, 4,733 patients with GCA, and 35,272 matched controls from the general population (Table 1). The incidence rate of any aortic complication per 1,000 person years was highest for GCA (11.69) followed by PMR (6.78) and the general population (5.09). Compared to patients with PMR, patients with GCA had a higher risk of any aortic complication (aHR 1.87, 95% confidence interval (CI) 1.54-2.17); the risk was similar for patients from the general population (aHR 0.95, 95% CI 0.84-1.06) (Figure 1). A sensitivity analysis of patients with PMR who developed GCA was also performed; as compared to patients with PMR-GCA, patients with GCA had a similar risk of any aortic complication (aHR 0.85, 95% CI 0.60-1.19); the risk was lower for patients from the general population (aHR 0.41, 95% CI 0.29-0.56) (Figure 2).
Conclusion: Patients with PMR had a lower risk of aortic complications as compared to patients with GCA and a similar risk as compared to those in the general population. Patients with PMR who were later diagnosed with GCA had a similar risk of developing aortic complications from that time point as compared to those who were initially diagnosed with GCA. Our results support the role of large vessel vasculitis screening in patients with GCA but not PMR.
To cite this abstract in AMA style:
Carlson K, Kaymakci M, Sattui S, Putman M. Incidence of Aortic Aneurysm, Dissection, or Rupture Among Patients with Polymyalgia Rheumatica and Giant Cell Arteritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/incidence-of-aortic-aneurysm-dissection-or-rupture-among-patients-with-polymyalgia-rheumatica-and-giant-cell-arteritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/incidence-of-aortic-aneurysm-dissection-or-rupture-among-patients-with-polymyalgia-rheumatica-and-giant-cell-arteritis/