Session Information
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
Background/Purpose: Several autoimmune diseases (AD) may be associated with interstitial lung disease (ILD), contributing to increased morbidity and mortality in these patients. We aimed to study the risk of ILD in different ADs and the impact of ILD on the outcomes of AD hospitalized patients utilizing the national inpatient sample database.
Methods: We used the national inpatient sample of 2016-2019 to identify patients with a concomitant discharge diagnosis of ILD and AD [systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), systemic sclerosis (SS), Sjogren’s syndrome (SJ), dermato-polymyositis (DM/PM), ANCA associated vasculitis (ANCA-V) or mixed connective tissue disorder (MCTD)] using ICD-10 codes. We divided patients into AD with ILD (AD+ILD) and AD without ILD (AD-ILD) groups. The two groups were compared for baseline characteristics, comorbidities, and outcomes. Univariate and multivariate regression analyses were done. We also calculated the odds of ILD in different ADs among all adult hospitalizations.
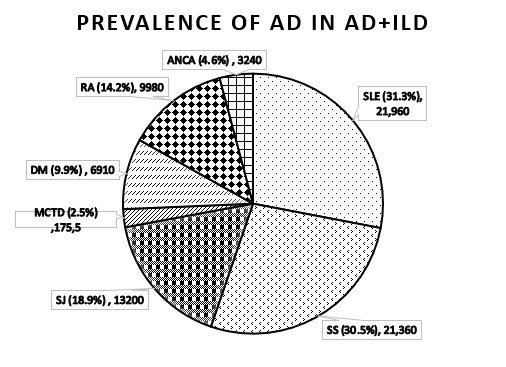
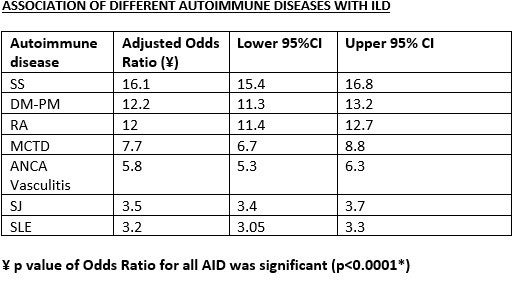
Results: Of 1,153,815 AD hospitalizations, 70,140 (6.1%) patients had concomitant ILD. Patients in the AD+ILD group were more likely to be older (mean age 63.8 vs 57.4 years), females (78.2% vs 21.7 %), Black (23.9% vs 22.8%)/ Hispanic ethnicity (12.8% vs 11.3%), and less likely to be Whites (56.2% vs 60.3%) than those in the AD-ILD group. TAD patients with ILD had higher rates of comorbid coronary artery disease (21% vs 17%), Obstructive sleep apnea(14% vs 9%), supplemental oxygen dependance (27.8% vs 4.6%) and pulmonary hypertension ( 3.9% vs 0.5%).The proportion of different ADs in AD+ILD hospitalizations is depicted in figure 1 and the odds of ILD in different ADs are depicted in Table 1. 4115 (2.5%) AD patients with ILD died during hospitalization (aOR=1.97, 95% CI=1.81 -2.15, p< 0.0001*). AD patients hospitalized with ILD were more likely to have secondary complications such as pneumonia (aOR 1.89, 95% CI 1.81-1.98), sepsis (aOR=1.23, 95% CI=1.14 -1.33), acute right heart failure (aOR 2.41, 95% CI 1.7-3.27), acute respiratory failure (aOR 2.9, 95% CI 2.78-3.05) and required mechanical ventilation (aOR 1.54, 95% CI 1.43-1.67) [p< 0.0001*]. ILD hospitalizations in ADs incurred higher hospitalization charges ($78,0006 vs $64,712) and longer length of stay (6.5days vs 5.4 days, p < 0.0001*).
Conclusion: SLE and systemic sclerosis were the most common ADs in adult ILD hospitalizations. ILD increased the risk of mortality by 2-fold in AD hospitalizations, along with several other complications and increased economic burden. Therefore, early recognition and treatment of ILD are recommended in ADs.
To cite this abstract in AMA style:
Kannayiram S, Arora S. In-hospital Outcomes of Autoimmune Diseases Complicated by Interstitial Lung Disease: A National Inpatient Sample Analysis [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/in-hospital-outcomes-of-autoimmune-diseases-complicated-by-interstitial-lung-disease-a-national-inpatient-sample-analysis/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/in-hospital-outcomes-of-autoimmune-diseases-complicated-by-interstitial-lung-disease-a-national-inpatient-sample-analysis/