Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Axial spondyloarthritis (axSpA) is often diagnosed late, while there is also a problem of over- and misdiagnosis in patients with chronic back pain. Imaging, especially magnetic resonance imaging (MRI), is important for diagnosis and differential diagnosis, but interpreting imaging findings in sacroiliac joints requires specific expertise.
The Improve-axSpA project was aimed to assess the effectiveness of telemedicine support in enhancing the diagnostic accuracy of patients suspected of having axSpA.
Methods: We established a central telemedicine platform that allowed the collection of clinical and imaging information from patients who presented to rheumatologists and orthopaedists with suspicion of axSpA. Participating centres were encouraged to recruit appropriate patients consecutively. Collected information included the suspected diagnosis and imaging findings, demographic and laboratory data, information on potential mechanical stress factors, characteristics of back pain and SpA features as assessed by the local physician. The central expert evaluation included detailed assessment of the submitted data including imaging and the final conclusion on the presence or absence of axSpA.
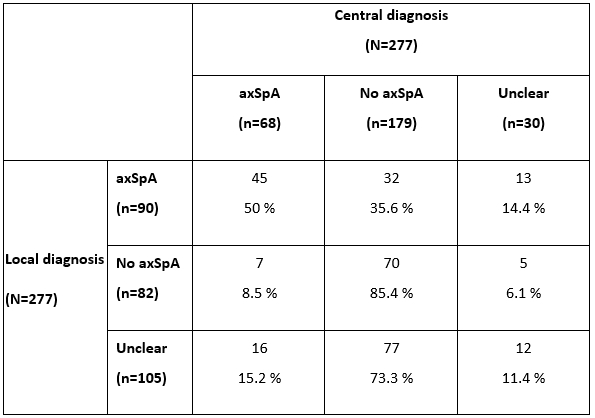
Results: A total of 25 study centres submitted 277 cases for the central evaluation until March 2023. The distribution of the diagnoses according to the local and central assessment is presented in table 1. A total of 90/277 patients (33%) were locally diagnosed with axSpA. Only in 45 (50%) of those cases axSpA could be confirmed after central evaluation, while in 32 patients (36%) an alternative reason of back pain (in the majority of cases – degenerative / mechanical disorders, non-specific back pain) were found to be more likely. In contrast, among 82 patients with no axSpA according to local assessment, in 70 (85%) of those patients axSpA could be excluded based on central evaluation. In 105 cases with inconclusive local diagnosis, axSpA was more frequently excluded than confirmed (73% vs. 15%). In a total of 30 patients, the diagnosis could not be finally determined after central assessment, this being related in most cases to insufficient imaging. Several important differences could be found between patients with centrally confirmed vs. excluded axSpA: patients without SpA were older, more often females (and more often with a history of pregnancies and 2 and more deliveries), had lower CRP, higher BMI and were less frequently HLA-B27-positive. At the same time, other SpA-characteristics including inflammatory back pain, as well as imaging characteristics as reported by the local rheumatologist were not discriminative between the groups. However, the presence or absence of SpA-compatible active inflammatory and structural changes on MRI of sacroiliac joints according to the central assessment were highly discriminative between the groups with confirmed and excluded SpA.
Conclusion: The Improve-axSpA interim analysis suggests a high risk of overdiagnosis of SpA in daily clinical practice. Telemedicine tools with central evaluation of clinical and imaging information may be helpful in the diagnostic process for patients with suspected axSpA.
To cite this abstract in AMA style:
Poddubnyy D, Kämmerer M, Kremers M, Schoppen B, Arens C, Wiedon A, Redeker I, Baraliakos X. Improving the Diagnostic Accuracy in Axial Spondyloarthritis: Interim Results of a Nationwide Telemedicine Project [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/improving-the-diagnostic-accuracy-in-axial-spondyloarthritis-interim-results-of-a-nationwide-telemedicine-project/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/improving-the-diagnostic-accuracy-in-axial-spondyloarthritis-interim-results-of-a-nationwide-telemedicine-project/