Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: No shows are a widespread problem across medical practices, and lead to negative consequences for patients and providers (Mendel 2017). The rheumatology division at our institution has an access problem, with wait time up to five months for new patient visits (NPVs). NPV no shows lead to wasted resources that negatively impact patient access. A root cause analysis suggested that the most common reason for patients no showing for NPVs was because they forgot about the appointment. In addition, most patients (54%) reported not receiving a reminder, despite the fact that our institution sends out automated robocalls 48 hours prior to all appointments.
Methods: We used the A3 model to conduct a quality improvement project to decrease the no show rates for NPVs. Baseline no show rates for our four clinical practice sites were determined, and the site with the highest baseline rate (PMUC) was selected for the intervention. We then conducted a pilot of manual phone call reminders two weeks prior to NPVs for two providers at the PMUC practice site. Data was obtained using EMR reports and analyzed using statistical process control charts.
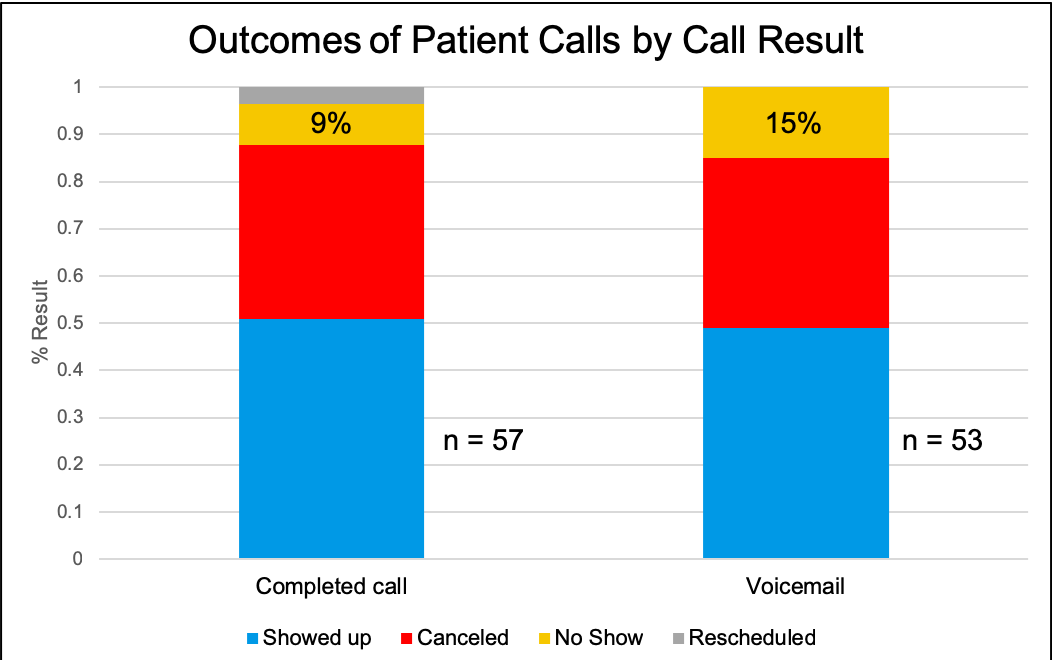
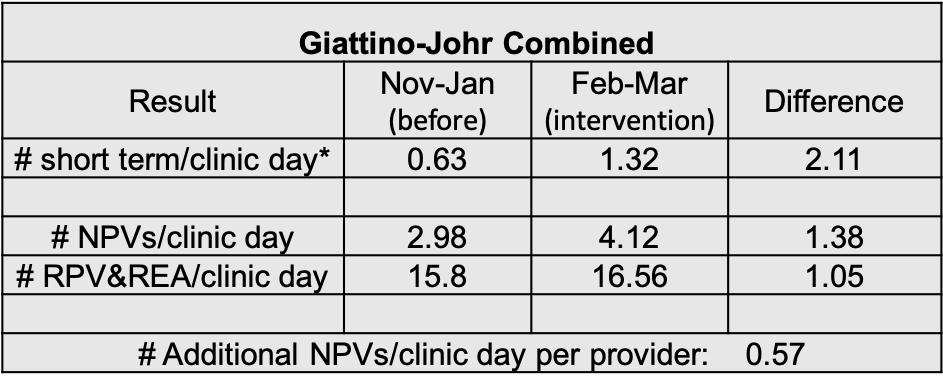
Results: Over the two month trial period, 110 patients were given manual phone call reminders. 57 patients had completed phone calls and 53 patients were left voicemails [Figure 1]. The no show rate for patients who had completed calls was lower than for those who were left voicemails (9% vs 15%) [Figure 1]. The no show rate for NPVs did not significantly decrease during the intervention period [Figure 2]. However, there was a nonsignificant decrease in the NPV no show rate from 20% to 15%. Secondary metrics to evaluate access were then assessed. The number of short term visits, defined as patients who had appointments made within one week of the visit date (typically patients off the waitlist), more the doubled during the intervention period [Table 1]. The total rate of NPVs seen by the two pilot providers increased by 38% [Table 1]. During the intervention period, an extra 0.57 NPVs were seen per provider per full clinic day, correlating with a revenue generation of about $100 per full provider clinical day.
Conclusion: We conducted a QI project that used manual phone call reminders to reduce the no show rate for NPVs at one of our clinical practice sites. While there was no significant decrease in the no show rate, the mean did decrease by 5% during the intervention period. Notably, there were more short term visits and an increase in the total NPV rate seen during the intervention period, suggesting improved access. The likely reason for the larger increase in access metrics compared to the no show rate is that the intervention resulted in earlier cancellations leading to an increased opportunity to schedule patients in those open appointment slots. Due to institutional policy, we were not able to adapt automated robocalls, and it is not clear if earlier robocalls would similarly lead to an increase in short term visits and improved access. Our QI project suggests that manually calling patients two weeks prior to their NPV appointments may help decrease the no show rate and likely results in improved access. The revenue generated by the increased productivity suggests this a cost-effective and sustainable change.
To cite this abstract in AMA style:
Zamore R. Improving Access in an Academic Rheumatology Department by Reducing the No Show Rate [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/improving-access-in-an-academic-rheumatology-department-by-reducing-the-no-show-rate/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/improving-access-in-an-academic-rheumatology-department-by-reducing-the-no-show-rate/