Session Information
Date: Sunday, November 17, 2024
Title: Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: ILD is the leading cause of mortality in patients with idiopathic inflammatory myopathies, and rapidly progressive ILD, associated mainly with anti-MDA5 antibody, is the most devastating subset with early mortality risk. We established a multicenter retrospective cohort of Japanese patients with myositis-ILD (JAMI), which enrolled 497 incident cases from 2011 to 2015. In this cohort, ~40% of anti-MDA5-positive patients died within 6 months. After the original JAMI era, clinical practice has changed significantly, with early recognition of anti-MDA5-positive patients and common use of initial combination therapy. We have launched a new cohort (JAMI2R) that retrospectively enrolled incident cases diagnosed between 2016 and 2020, and a prospective registry (JAMI2P) enrolling newly diagnosed patients since 2021. This study investigated survival trends in patients with myositis-ILD over the last decade using three cohorts with different time periods of diagnosis.
Methods: The eligible patients were selected from JAMI (2011-2015), JAMI2R (2016-2020), and JAMI2P (2021-) based on age at onset ≥16 years; satisfaction of the ACR/EULAR classification criteria; ILD confirmed by high-resolution CT; and availability of follow-up data for ≥1 year except mortality event. Kaplan-Meier analysis with log-rank test was used to compare the equality of survival curves for individual groups. The cause-specific Cox proportional hazards model was used for multivariate analysis to identify an optimal model for predicting mortality.
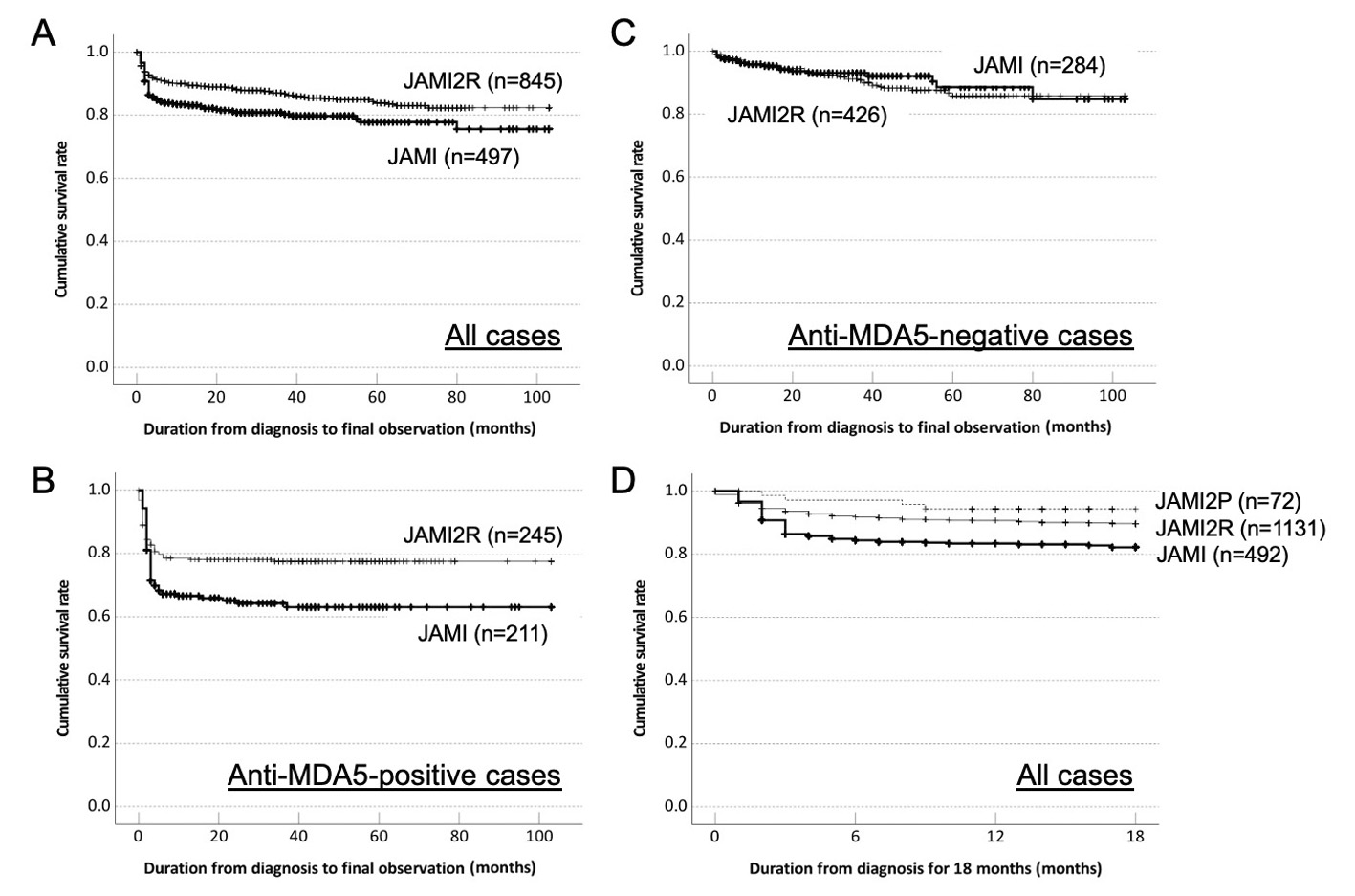
Results: Of 497, 1151, and 321 patients enrolled in JAMI, JAMI2R and JAMI2P, 497, 1131, and 72 were eligible for the analysis, respectively. Because the number of eligible patients for JAMI2P was smaller and their observation period was much shorter than other cohorts, primary analysis was conducted by comparing survivals between JAMI and JAMI2R. Cumulative survival rates were better in JAMI2R than JAMI (P=0.002; Fig 1A). Improved survival was observed in anti-MDA5-positive group, but not in anti-MDA5-negative group (Fig 1BC). Focused on early mortality, there was a trend toward better survivals over 18 months in JAMI2P than other cohorts (Fig 1D). As a cause of mortality, ILD-related respiratory insufficiency decreased with time; 82% in JAMI, 46% in JAMI2R, and 25% in JAMI2P. A multivariable regression model confirmed that the time period of diagnosis (JAMI2R versus JAMI) was identified an independent factor for a better survival even after adjustment for clinically relevant baseline confounders, such as age at onset and requirement of oxygen supplementation (hazard ratio 0.6, 95% confidence interval 0.4-1.0, P=0.03), while diagnosis period was no longer prognostic when treatment regimens were included in explanatory variables for the analysis.
Conclusion: The survival of patients with myositis-ILD, especially those with anti-MDA5, had improved over the last 10 years. This was attributable to decrease in early mortality due to rapidly progressive ILD, and might be associated with refinement of the treatment strategy.
To cite this abstract in AMA style:
Kuwana M, Masui K, Kawakami A, Suda T, Sato S, Kawaguchi Y, Johkoh T, Hoshino T, Shimada N, Kondoh Y, Tanino Y, Takeuchi T, Abe Y, Kimura N, Inoue Y, Tomii K, Arai T, Yamaoka K, Sasaki K, Naniwa T, Nakashima R, Shima K, Nishiyama O, Waseda Y, Mukae H, Chiba H, Ikeda K, Ichikado K, Kirino Y, Amano K, Nawata T, Kishaba T, Asatori D, Kobayashi D, Gono T. Improved Survival in Patients with Myositis-Associated Interstitial Lung Disease (ILD) During the Period 2011 to 2023: Comparative and Integrative Analysis of Three Multicenter Cohorts in Japan [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/improved-survival-in-patients-with-myositis-associated-interstitial-lung-disease-ild-during-the-period-2011-to-2023-comparative-and-integrative-analysis-of-three-multicenter-cohorts-in-japan/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/improved-survival-in-patients-with-myositis-associated-interstitial-lung-disease-ild-during-the-period-2011-to-2023-comparative-and-integrative-analysis-of-three-multicenter-cohorts-in-japan/