Session Information
Date: Monday, November 13, 2023
Title: (1082–1099) Measures & Measurement of Healthcare Quality Poster I
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: We embedded a clinical pharmacist into our university rheumatology clinics beginning in June 2022 to improve patient experience and reduce provider burden based on projected improved medication access and improved organizational financial health. The objective was to demonstrate how implementing a rheumatology clinical pharmacist with a medication access team can impact patient, provider, staff, and pharmacy outcomes.
Methods: In this mixed methods study at two academic clinics in 2022-23, we employed pre-post surveys and electronic health record (EHR) data review. We conducted a pre-implementation pharmacy services satisfaction survey and baseline needs assessment with providers and clinical staff to set priorities and leveraged existing patient surveys pre-post. Based on survey results, we categorized outcome measures of clinical pharmacist and medication access team impact into four groups: patient, provider, clinic staff, and pharmacy. EHR data included prior authorization quantity and turnaround time, manufacturer assistance referrals, time to infusion, and number of new patient enrollments, and prescriptions captured within the organizational specialty pharmacy. At six-months post-implementation, providers and clinic staff were asked to complete a post-implementation survey to assess the impact of the embedded clinical pharmacist.
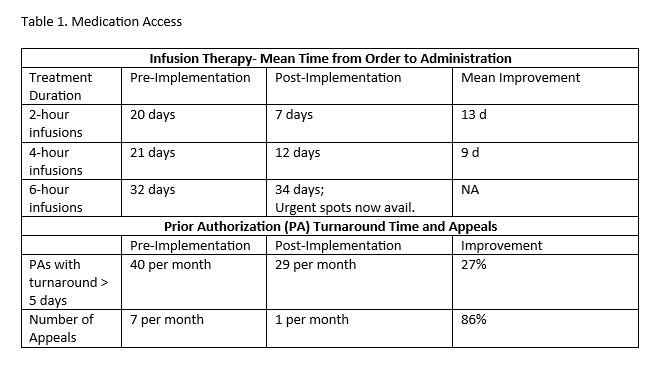
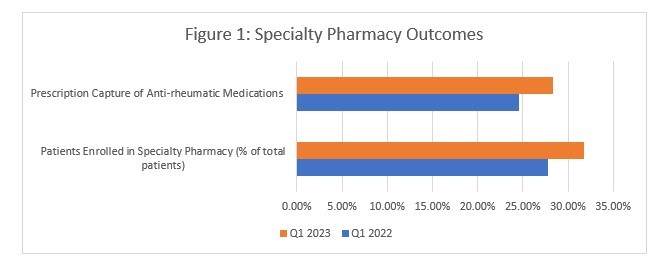
Results: Patient and EHR data showed improvement after the clinical pharmacist joined the rheumatology clinic team. When asked “How well the staff worked together to care for you?” 83.3% after vs. 77.2% baseline (Q2 2022 n=298 vs. Q2 2023, n = 277) responded “extremely well” (p=0.047). The time from order to infusion decreased 9-13 days for infusions of 4 hours or less (Table 1). Prior authorizations with a turnaround time greater than 5 days decreased by 27% (from 40 to 29/month); prior authorizations resulting in appeal decreased by 86% (from 7 to 1/month, Table 1). Our medication assistance program assisted many more patients (n=55 over 6 months) in obtaining medications through free drug programs. Prescription capture rate increased by 15% and patients enrolled in our specialty pharmacy increased from 27.8% (204/734) in Q1 2022, to 31.8% (228/718) in Q1 2023 (Figure 1).
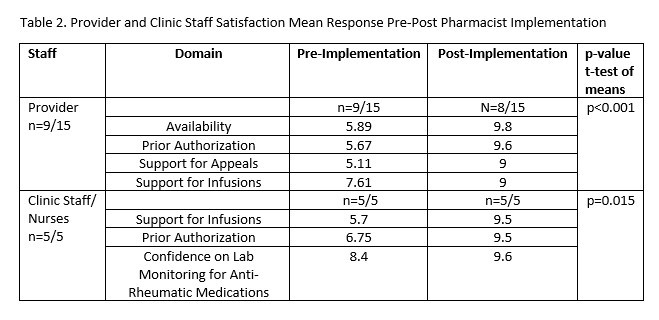
Provider and staff satisfaction also significantly improved. All provider items on medication communication, prior authorization assistance, and support for appeals and infusions rose (Table 2, p< 0.001). Clinic staff satisfaction also improved in the prior authorization process (mean 9.5 vs 6.75 on scale of 1-10 best) and support for infusions (5.7 vs 9.5; pooled p=0.015,). Nurses also reported being more comfortable on anti-rheumatic medication lab monitoring after education from our clinical pharmacist.
Conclusion: The addition of an embedded rheumatology clinical pharmacist with direct support from a medication access team has improved patient, provider, and clinical staff satisfaction and outcomes. Specialty pharmacy prescription capture improved, and the cost to support the position was covered by improved financial outcomes.
To cite this abstract in AMA style:
Gomez S, Ludwig T, Hartkopf K, Ferguson S, Zemlicka L, Jones M, Bartels C. Improved Patient and Team Satisfaction and Pharmacy Outcomes After Implementing a Rheumatology Clinical Pharmacist in a Large Academic Medical Center [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/improved-patient-and-team-satisfaction-and-pharmacy-outcomes-after-implementing-a-rheumatology-clinical-pharmacist-in-a-large-academic-medical-center/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/improved-patient-and-team-satisfaction-and-pharmacy-outcomes-after-implementing-a-rheumatology-clinical-pharmacist-in-a-large-academic-medical-center/