Session Information
Date: Sunday, October 21, 2018
Title: Rheumatoid Arthritis – Diagnosis, Manifestations, and Outcomes Poster I: Comorbidities
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Atherosclerotic plaque calcification is considered a stabilizing physiologic process; calcified coronary plaques (CP) are less prone to rupture and yield lower risk of cardiovascular events compared to non-calcified (NCP) or the more vulnerable partially calcified, mixed plaques (MP). Interestingly, higher coronary artery calcium score (CACS) and its progression associate with higher event risk in general patients. Likewise, we reported that CACS predicted cardiac events in rheumatoid arthritis (RA) patients independently of risk factors or cardiac risk scores. To address this paradox, we evaluated the contribution of MP burden to CACS as well the influence of change in MP burden on CACS progression in RA patients with a baseline and follow-up evaluation of coronary anatomy with computed tomography angiography (CCTA).
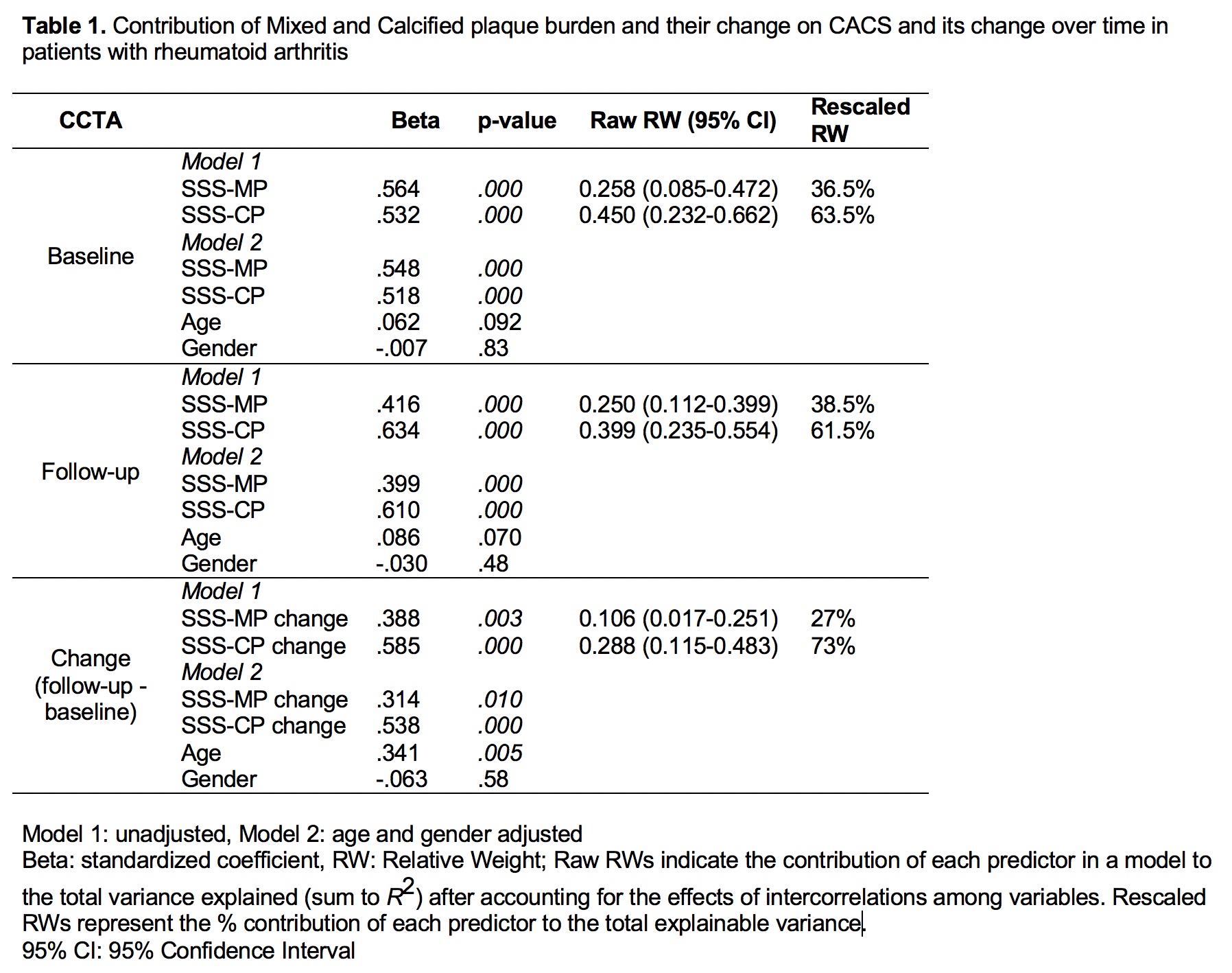
Methods: Ninety-nine patients underwent a repeat CCTA within 83±3.6 months from baseline. Total number of segments with plaque (segment involvement score-SIS) and cumulative stenosis severity rendered by plaque over all evaluable segments (segment stenosis score-SSS) we computed for all participants. Coronary lesions were defined as non-calcified (NCP), mixed (MP) or calcified (CP). Generalized Linear Models predicted the contribution of MP and CP plaque burden to the baseline and follow-up CACS as well as the influence of change in the burden of the respective lesions on CACS progression.
Results: Mixed and calcified plaque burden (SSS-MP and SSS-CP respectively) strongly correlated with CACS at both baseline (rmp= 0.75 and rcp= 0.77, p<0.001) and follow-up (rmp= 0.57 and rcp= 0.68 , p<0.0001), whereas non-calcified plaque did not (rncp= -0.03, p=0.85 and -0.16, p=0.30 respectively). Both MP and CP burden comparably and significantly contributed to CACS magnitude at both times; MP accounted for 36.5% and 38.5% of explainable variance in CACS while CP accounted for 63.5% and 61.5% of it at baseline and follow-up respectively. Likewise, change in MP and CP burden from baseline to follow-up significantly contributed to and justified 27% and 73% of explainable CACS change variance respectively.
Conclusion: The vulnerable MP and the more stable CP burden and their change significantly and collectively contributed to CACS at any time as well its progression respectively in patients with RA. Therefore, the MP burden and its change epitomize the vulnerability components within the higher baseline and progressing CACS scores yielding higher cardiovascular event risk.
To cite this abstract in AMA style:
Karpouzas G, Ormseth S, Hernandez E, Budoff M. Implications of Coronary Artery Calcium Score and Its Change over Time As Markers of Coronary Plaque Vulnerability and Patient Risk in Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/implications-of-coronary-artery-calcium-score-and-its-change-over-time-as-markers-of-coronary-plaque-vulnerability-and-patient-risk-in-rheumatoid-arthritis/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/implications-of-coronary-artery-calcium-score-and-its-change-over-time-as-markers-of-coronary-plaque-vulnerability-and-patient-risk-in-rheumatoid-arthritis/