Session Information
Date: Friday, November 6, 2020
Title: RA – Diagnosis, Manifestations, & Outcomes I: Pre-Onset & Early RA (0479–0483)
Session Type: Abstract Session
Session Time: 3:00PM-3:50PM
Background/Purpose: The aim of rheumatoid arthritis (RA) treatment is to target remission or at least low disease activity (LDA). We previously showed that SDAI remission at one year decreased the risk of 3-year structural progression in RA compared to patients in LDA.
The aim of the study was to compare 10-year severity outcomes including structural progression, function and orthopaedic surgery in RA patients with sustained remission versus patients with sustained LDA.
Methods: Patients: 813 patients with DMARDs-naïve early arthritis were included in the ESPOIR cohort and followed for 10 years. We analyzed data from with disease activity scores available at least at 6 visits out of 11 (n=523 with SDAI scores and n=527 with DAS28 scores).
Data analyzed: Remission was defined by SDAI ≤ 3.3 or DAS28< 2.6; LDA by 3.3 < SDAI score ≤ 11 or 2.6 ≤ DAS28 ≤ 3.2. Radiographs were centrally scored using the Total Sharp Score modified by Van der Heijde (mTSS) at baseline and at 10-year visits. Health Assessment Questionnaires (HAQ) and RA orthopaedic procedures were collected at each visit.
Analysis: patients were classified in 3 groups according to the SDAI at each visit between 1-year and 10-year visits. Group 1: patients with sustained SDAI remission. Group 2: patients with sustained SDAI LDA. Group 3: patients with moderate or high sustained disease activity. Patient with instable disease activity over time were excluded. A process latent mixed model were used to assess the impact of SDAI status over time on mTSS progression and mHAQ-DI evolution until 10-year visit was performed. A Cox proportional model was used to assess the impact of SDAI status over time on the risk of surgery. The following cofounding factors were included in the model: age, gender, disease duration, clinical center, erosions at baseline, ACPA positivity and titer , smoking habits, DMARDs use, time to start DMARD, biologic agents use and glucocorticoid use. Comparisons between remission and LDA fort the 3 outcomes over 10 years were obtained from the multivariate model with contrasts method. Analyses were repeated using DAS28.
Results: After classification of patients according to SDAI over time, group 1 included 48 patients in remission (9.2%), and group 2 included 135 patients in LDA (25.8%), while 79 patients (14.9%) could be classified in remission group 1 and 53 patients (10.1%) could be classified in LDA group 2 using the DAS28.
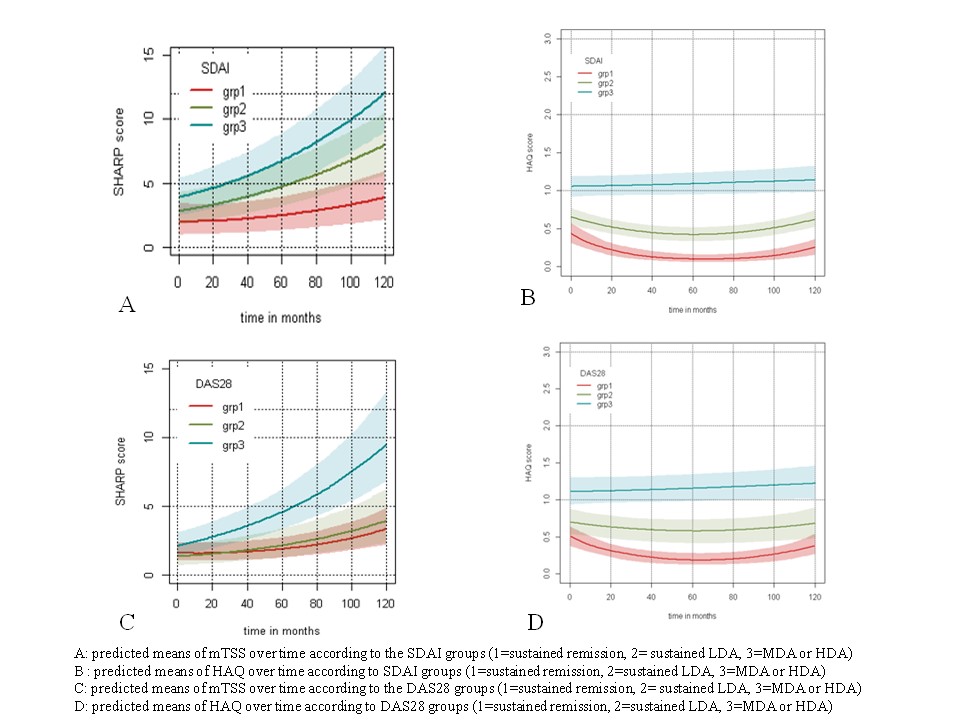
Patients with sustained SDAI remission had lower 10-year structural progression compared to patients in LDA (p=0.0014) and lower 10-year HAQ means (p< 0.0001). After 10 year follow-up only 53 patients have undergone orthopaedic procedures (10%) of whom 3 were in the group 1 according to SDAI and 14 in group 2 (p=0.14). When using DAS28 as disease activity score to classify patients, we identified a lower structural progression in the sustained DAS28 remission group compared to the LDA group (p=0.02) and patients in remission had lower 10-year HAQ means (p=0.0008) (figure), while no difference was observed for the risk of orthopaedic procedures between groups.
Conclusion: Aiming for SDAI or DAS28 remission rather than LDA during monitoring leads to better radiographic and functional outcomes at 10 years in early RA patients.
To cite this abstract in AMA style:
Dupont J, Guernec G, Degboé Y, Lioté F, Vittecoq O, Constantin A, Ruyssen Witrand A. Impact of Targeting Remission or Low Disease Activity on 10-year Severity in Rheumatoid Arthritis : Data from ESPOIR Cohort [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/impact-of-targeting-remission-or-low-disease-activity-on-10-year-severity-in-rheumatoid-arthritis-data-from-espoir-cohort/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-targeting-remission-or-low-disease-activity-on-10-year-severity-in-rheumatoid-arthritis-data-from-espoir-cohort/