Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Rheumatic diseases, such as rheumatoid arthritis (RA), psoriatic arthritis (PA), and systemic lupus erythematosus (SLE) can significantly impact quality of life. This burden extends beyond physical limitations as there is a well-established co-occurrence between rheumatic diseases and major depressive disorder (MDD). Understanding the relationship is crucial as effective management of RA, PA and SLE can improve MDD symptoms and vice versa. The purpose of this evaluation was to identify if well-controlled RA, PSA, or SLE are associated with improvements in MDD outcomes.
Methods: This was a cohort evaluation of commercial fully-insured and Medicare members of a large national health plan between 1/1/2018 and 1/1/2024. Members ≥ 18 years old were included if they had at least 2 claims for RA (ICD-10 code: M05 or M06), PSA (L40.5), or SLE (M32) during the evaluation period and at least 2 claims for MDD (F30-4 or F39). Members were excluded if they did not maintain continuous eligibility for 6 months before or after entrance into the study, had multiple conditions of interest, or had missing socioeconomic status (SES) data. The primary outcomes were the number of MDD claims and changes in antidepressant medication. Members were stratified into two groups: rheumatologic therapy changes or stable (i.e., no changes) therapy during the evaluation period; serving as a proxy for disease control. Continuous variables were assessed with the independent t-test or Mann-Whitney U test; categorical variables were assessed with the ꭓ2 test. Bivariate and multivariate logistic and Poisson regression assessed correlations between variables and outcomes; p-values < 0.05 were significant.
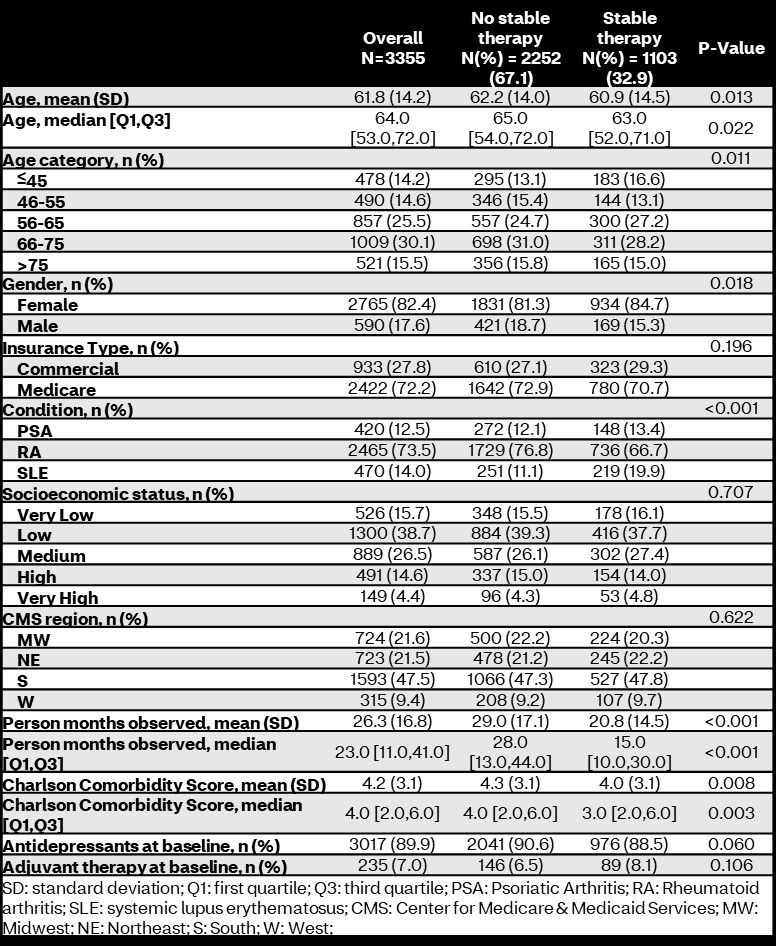
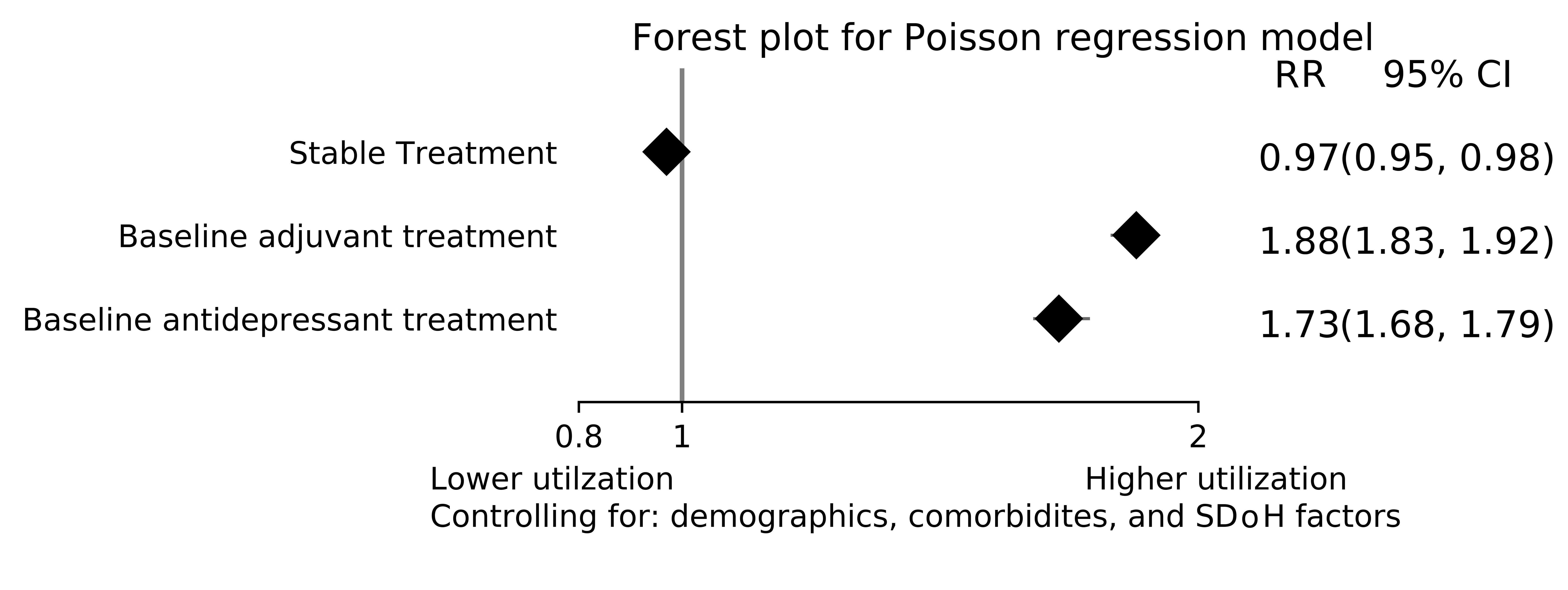
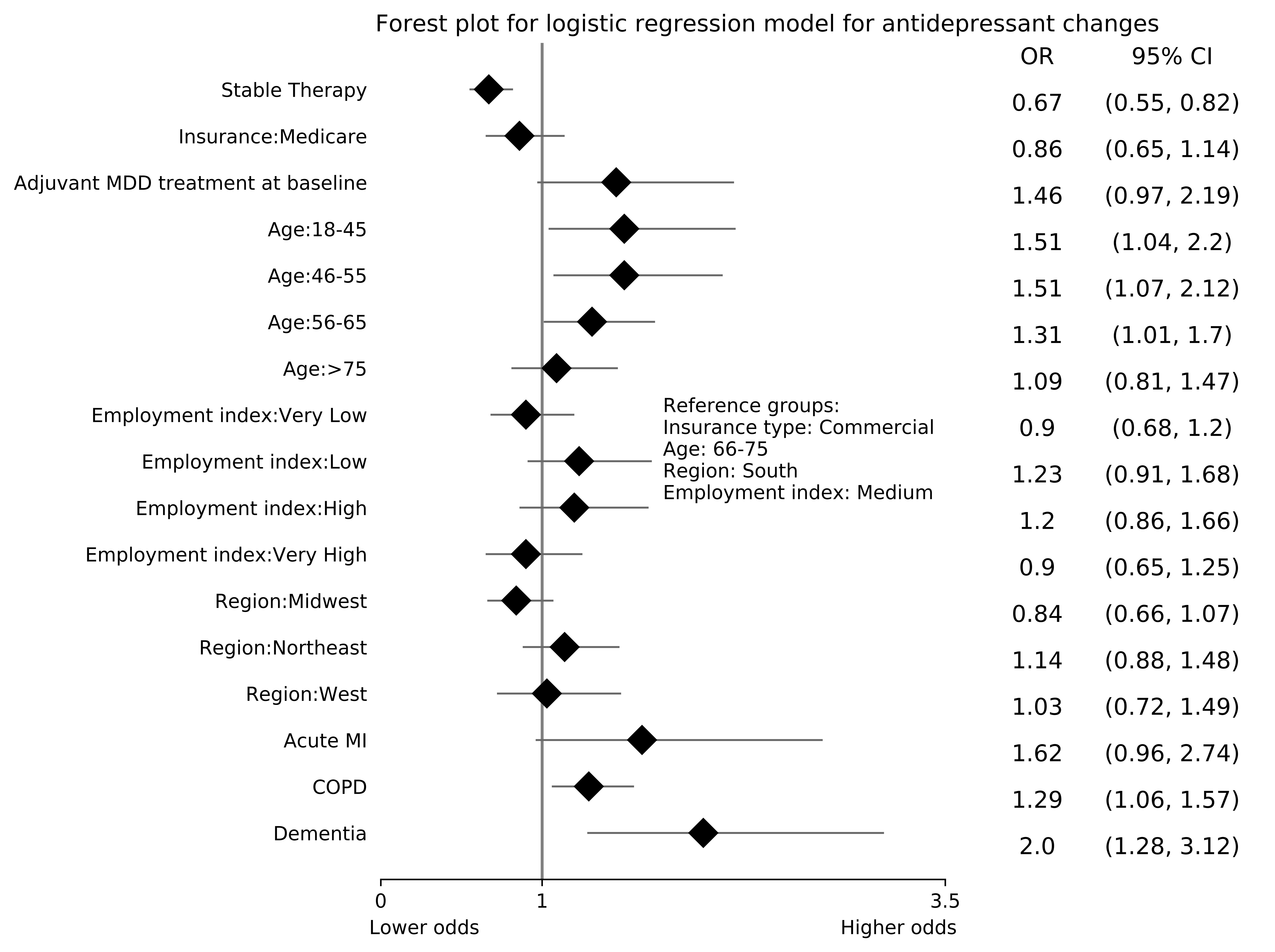
Results: In total, 3,355 members were included in this evaluation with 1,103 (32.9%) experiencing stable therapy. Members with stable therapy were younger, more likely to be female, less likely to have RA, and had fewer comorbidities, and were observed for less time than those with therapy changes (Table 1). No differences were found in baseline MDD therapy or SES. Unadjusted MDD claims rates were higher in the stable therapy group (12,494.6 vs. 9,403.2 MDD claims/1,000 person-years; incidence rate ratio: 1.33 [95% confidence interval (CI): 1.31-1.35]; p< 0.0001). After adjusting for demographic, comorbidity, and social determinants of health confounders, members in the stable therapy group had lower rates of MDD care utilization (rate ratio [95% CI]: 0.97 [0.95-0.98]; p< 0.0001; Figure 1). Members with stable therapy experienced less antidepressant medication changes (78.6% vs. 84.3%; p< 0.0001). After controlling for confounders, stable therapy members had lower risk of experiencing a medication change (odds ratio [95% CI]: 0.67 [0.55-0.82]; p< 0.0001) compared to those with therapy changes (Figure 2).
Conclusion: Members with stable rheumatologic therapy had lower MDD-related care utilization and lower odds of experiencing antidepressant medication changes. These findings suggest that well controlled RA, SLE, or PSA appear to improve MDD outcomes.
To cite this abstract in AMA style:
Park J, Rutter C, Avalos-Reyes E, Anderson M, Cavers W, Verbrugge D, Johnson K. Impact of Stable Rheumatologic Therapy on Outcomes of Depression in Members with Rheumatoid Arthritis, Psoriatic Arthritis, and Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/impact-of-stable-rheumatologic-therapy-on-outcomes-of-depression-in-members-with-rheumatoid-arthritis-psoriatic-arthritis-and-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-stable-rheumatologic-therapy-on-outcomes-of-depression-in-members-with-rheumatoid-arthritis-psoriatic-arthritis-and-systemic-lupus-erythematosus/