Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose : We surveyed adult patients with a history of pediatric systemic lupus erythematosus (pSLE) regarding their process of transition from pediatric to adult care to determine if social and psychological constructs influence patients’ perception of transition preparedness.
Methods : Surveys were both mailed and administered in clinic to adult patients with pSLE seen in an adult SLE clinic. Demographics including sex, race, age, employment (full time, part time, not working) marital status (single, married, partnered, divorced) and education level (< high school, high school, college degree, graduate degree) were collected. Patients reported preparedness for transition as: completely prepared, mostly prepared, neutral, mostly unprepared or completely unprepared. The modified Medical Outcomes Study Social Support Survey (mMOS SS, range 8-40 points, higher scores indicate more support) and the Brief Illness Perception Questionnaire (IPQ, range 0-80 points, higher scores indicate increased perceptions of illness) were completed. We calculated Spearman rank correlations between variables and self-reported transition preparedness. Discrimination was assessed with the receiver-operating characteristic (area under the curve, AUC). Two multivariable logistic regression models, each including race, marital and employment status, educational level, and mMOS SS in one model and IPQ in the other, were analyzed to identify factors associated with transition preparedness.
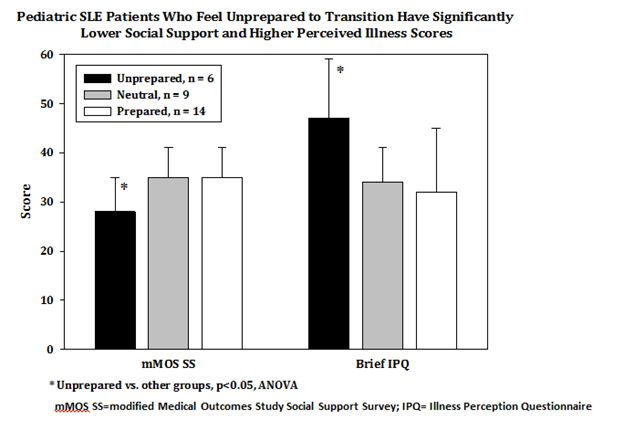
Results : Of 258 surveys distributed, 30 patients (12%) responded. Average age was 28 ± 5 years, (range 21-38), 27 (90%) were female. The cohort was 60% (n=18) white, 10% (n=3) black, 10% (n=3) Hispanic and 17% (n=5) Asian. Twenty subjects (67%) were single, 67% were employed full time and 67% had a college degree. Fourteen subjects (47%) reported feeling completely or mostly prepared, 9 (30%) were neutral and 6 (20%) felt mostly or completely unprepared for transition. Higher social support per the mMOS SS was positively correlated with preparedness (Spearman rho= 0.42, p=0.02). Prepared subjects (n=14) vs. unprepared subjects (n=6) had significantly higher mMOS SS scores (35 ±6 vs. 28±7, p=0.02); AUC =0.83. In a multivariable model, high mMOS SS scores were predictive of preparedness (p=0.03). In contrast, high IPQ were negatively correlated with preparedness (Spearman rho= -0.48, p<0.01). Mean IPQ scores were significantly lower in prepared vs. unprepared patients (32±13 vs. 47±12, p=0.02); AUC=0.76. Lower IPQ scores were predictive of preparedness in the multivariable model (p=0.02).
Conclusion : In an adult group of pSLE patients, self-reported lack of preparedness for transition was strongly associated with low social support and increased cognitive and emotional representations of illness. The transition from pediatric to adult care for SLE may be improved by implementing appropriate support systems.
To cite this abstract in AMA style:
Son MB, Zurakowski D, Kreps DJ, Case S, Costenbader KH. Impact of Social Support and Illness Perception on the Transition of Pediatric SLE Patients to Adult Care [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/impact-of-social-support-and-illness-perception-on-the-transition-of-pediatric-sle-patients-to-adult-care/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-social-support-and-illness-perception-on-the-transition-of-pediatric-sle-patients-to-adult-care/