Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Factors influencing optimal medication adherence in members with rheumatoid arthritis (RA), psoriatic arthritis (PA), or systemic lupus erythematosus (SLE) are poorly understood. This evaluation sought to examine the relationship between gender and medication adherence. As a secondary aim, the association of additional clinical and sociodemographic characteristics on primary outcomes were also explored.
Methods: This was a cohort study of commercial fully-insured and Medicare Advantage members of a large national health plan. Members ≥18 years old were included if they had at least 2 claims for RA (ICD-10 code: M05 or M06), PSA (L40.5), or SLE (M32) during the evaluation period (1/1/2018 to 1/1/2024). Members were excluded if they did not maintain continuous eligibility for 6 months before or after entrance into the evaluation, had >1 included condition or missing socioeconomic status (SES) data. Members were stratified by self-reported gender. Adherence to disease-modifying antirheumatic drugs (DMARD) was measured with proportion of days covered (PDC), calculated as the number of days with medication available divided by the number of days elapsed between the first fill and the calculated date of exhaust of the last fill in the evaluation period. Optimal adherence was defined as a PDC ≥0.8. Continuous variables were assessed with an independent t-test or Mann-Whitney U test; categorical variables were assessed with the ꭓ2 test. Adherence was evaluated using logistic regression; significant factors were included in the final multivariate model. Models were compared with the Akaike information criterion (AIC) and selected to balance AIC and overall interpretability; p-values < 0.05 were significant.
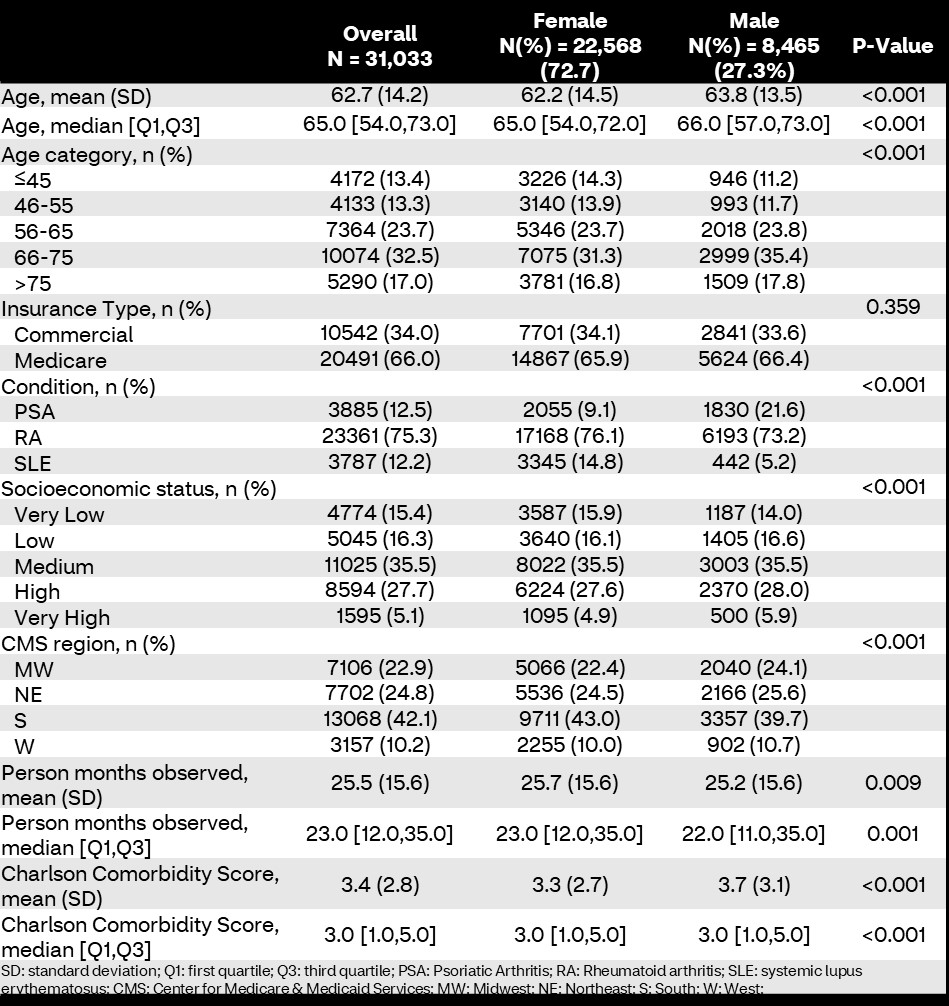
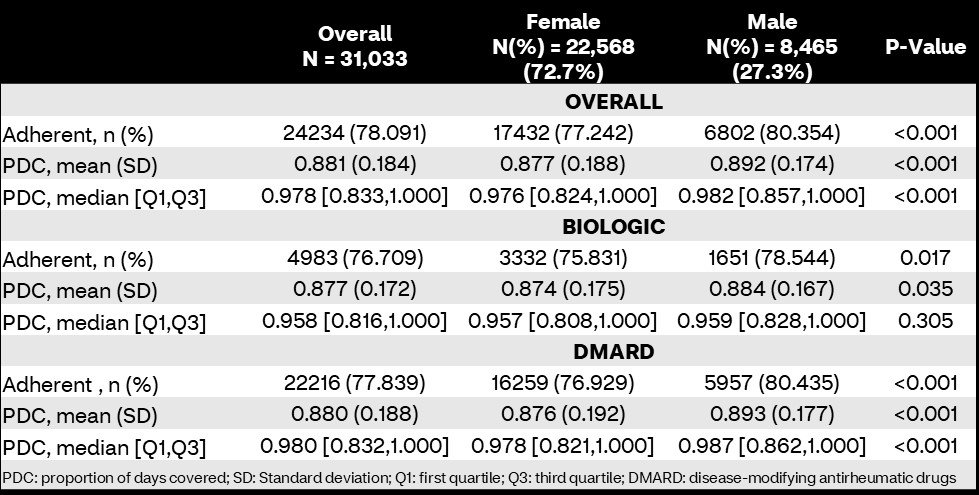
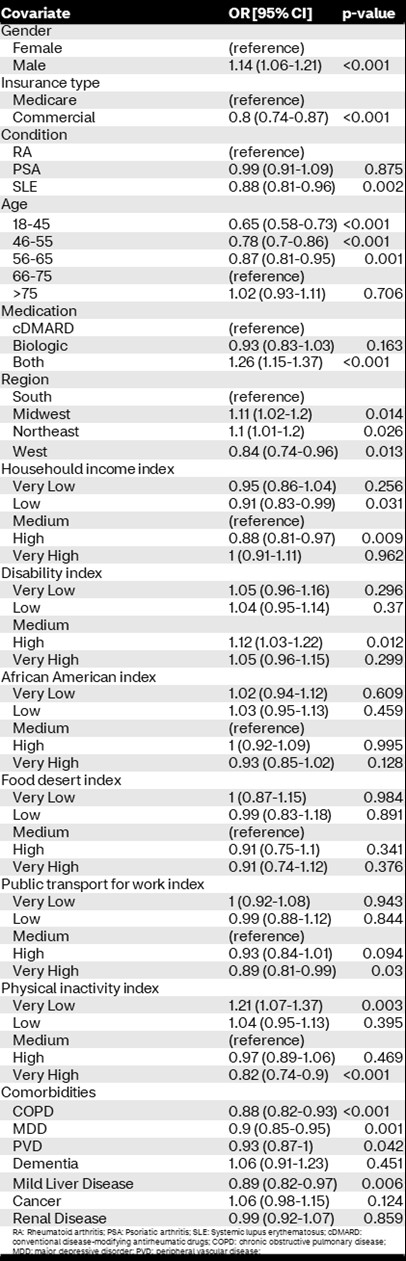
Results: 31,033 members were included; 8,465 (27.3%) identified as male. Males tended to be older, had more comorbidities, reside in higher SES zip codes, resided in Southern regions, have shorter observation time, and more likely to have PSA compared to females, all p< 0.05 (Table 1). Adherence was high in this cohort (mean PDC 88.1%, proportion adherent 78.1%); however, males were more adherent than females (80.3% vs. 77.2%, p< 0.001) with higher mean PDC (89.2 [standard deviation 17.4] vs. 87.7 [18.8]; p< 0.001). Similar results were seen between conventional and biologic DMARD specific adherence (Table 2). Controlling for confounding variables, male gender was associated with higher odds of medication adherence compared to female gender (odds ratio [OR]: 1.14 [95% confidence interval: 1.06-1.21]; p < 0.001). Other factors associated with increased odds of adherence include receiving both biologic and conventional DMARDs during the evaluation period, residing in Midwest or Northeast regions, and living in a zip code with high disability or very low physical inactivity indices (Table 3).
Conclusion: Male members with RA, SLE, and PSA had higher medication adherence than female members. Other factors associated with medication adherence included age, medication type, geographic location, and social determinants of health indices.
To cite this abstract in AMA style:
Park J, Rutter C, Avalos-Reyes E, Anderson M, Cavers W, Verbrugge D, Johnson K. Impact of Sex on Medication Adherence in Members with Rheumatoid Arthritis, Psoriatic Arthritis, or Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/impact-of-sex-on-medication-adherence-in-members-with-rheumatoid-arthritis-psoriatic-arthritis-or-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-sex-on-medication-adherence-in-members-with-rheumatoid-arthritis-psoriatic-arthritis-or-systemic-lupus-erythematosus/