Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Observational studies on RA therapeutic classes have shown conflicting results on their impact on mortality and cancer. When analyzing long-term outcomes, it is essential to account for changes in patient treatment over time. We assessed the association between RA therapeutic classes and risk of all-cause mortality and cancer in a large, population-based RA cohort.
Methods: Patients with RA were identified from the Ontario Rheumatoid Arthritis Database (ORAD), a population-based registry derived using a validated algorithm and maintained at ICES. We included individuals aged >67 years diagnosed between January 1, 2008, and December 30, 2013, and followed them through to December 30, 2023, with a minimum of 6 months follow-up. The outcomes of interest were all-cause mortality and health care utilization due to all-cause cancer requiring hospital admission, emergency department (ED) visits, or physician encounters. RA therapeutic class was treated as a time-varying exposure and categorized into 4 mutually exclusive groups: (1) No csDMARDs or AT use, (2) oral glucocorticoid (GC) use, (3) csDMARDs use only (reference), or (4) AT use (with or without csDMARDs). Given that CVD is the leading cause of death in RA and shares risk factors with cancer, the cohort was stratified by CVD risk at RA diagnosis. High-risk patients had established CVD, diabetes, or hypertension. Associations between treatment class and outcomes were evaluated using the Andersen-Gill Cox model, adjusted for baseline covariates and csDMARD use.
Results: A total of 10,020 RA patients (mean age 75.5 years; 67.3% female) were included in the study. Of these, 80% were classified as high CVD risk and 20% as low CVD risk. Over a median follow-up period of 9.4 years, there were 5,004 deaths and 1,762 cancer events in the high-risk group, compared to 845 deaths and 436 cancer events in the low-risk group. In the high-risk group, no csDMARD/AT use (HR: 2.37) and oral GC use (HR: 2.32) were significantly associated with increased all-cause mortality, while AT use was associated with a lower mortality hazard (Table). Similar findings were seen in the low-risk cohort. Lack of csDMARD/AT use was associated with a higher likelihood of cancer-related hospitalizations or visits in both high and low CVD risk groups (Table).
Conclusion: In this population-based cohort of older RA patients, treatment choice was significantly associated with mortality hazard. Advanced therapies were protective, while GC use and lack of RA treatment were associated with higher mortality. RA treatment had no significant impact on cancer hazard.
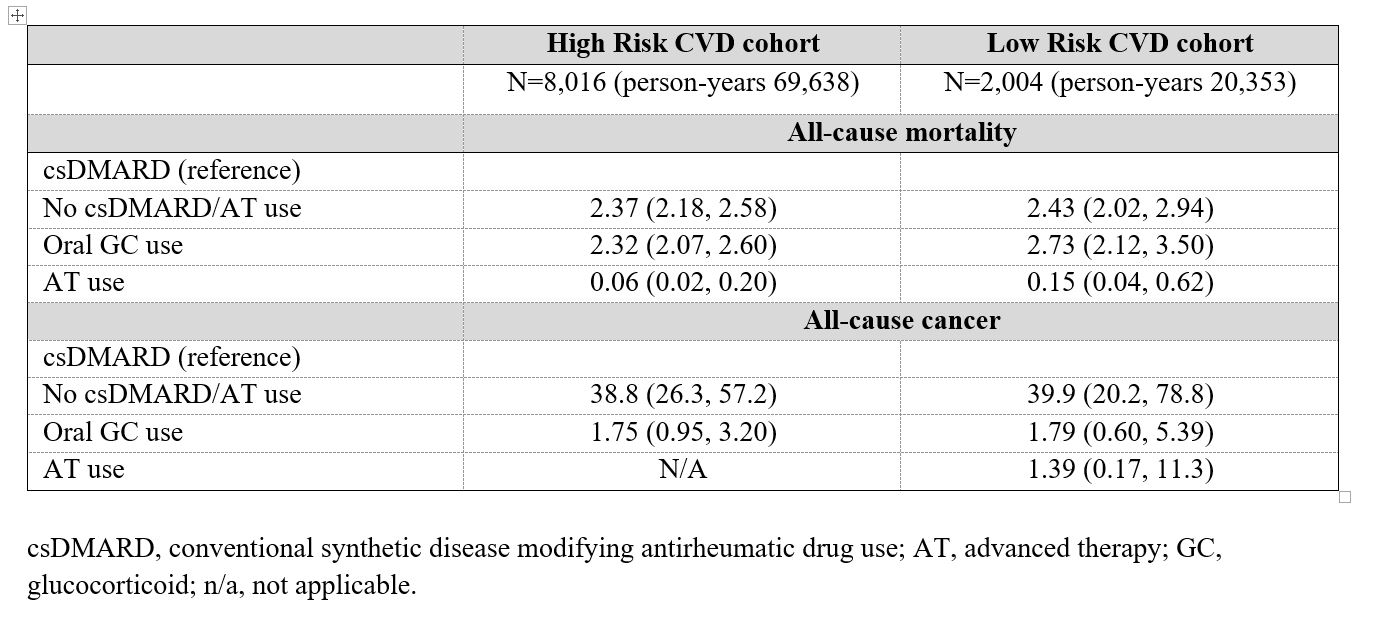 Table. Adjusted hazard ratios (HR) and 95% confidence intervals for all-cause mortality or all-cause cancer by RA therapeutic class and baseline cardiovascular (CVD) risk.
Table. Adjusted hazard ratios (HR) and 95% confidence intervals for all-cause mortality or all-cause cancer by RA therapeutic class and baseline cardiovascular (CVD) risk.
To cite this abstract in AMA style:
Movahedi M, Cesta A, Aydin S, Akhavan P, Kendzerska T, Bombardier C, Kuriya B. Impact of Rheumatoid Arthritis Therapeutic Classes on Risk of All-Cause Mortality and All-Cause Cancer: A Population-Based Cohort Study [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/impact-of-rheumatoid-arthritis-therapeutic-classes-on-risk-of-all-cause-mortality-and-all-cause-cancer-a-population-based-cohort-study/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-rheumatoid-arthritis-therapeutic-classes-on-risk-of-all-cause-mortality-and-all-cause-cancer-a-population-based-cohort-study/
