Session Information
Session Type: Poster Session A
Session Time: 1:00PM-3:00PM
Background/Purpose: Due to its range of manifestations and lack of specific findings, early diagnosis of SLE is often a challenge, and serious complications, including LN, can occur. Of importance, SLE disproportionally affects women—more specifically, women of color.1 These individuals often suffer higher disease severity and mortality rates and are more likely to have multiple comorbidities and worse health-related quality of life.1 Recently, new drugs with the potential to positively impact disease and patient outcomes either have received FDA approval for the treatment of SLE and LN or are in late-stage development. As a result, clinicians require education regarding timely diagnosis and screening, current and emerging therapies, and strategies for reducing health disparities, especially in women of color. Equipped with this information, clinicians will be better prepared to help patients achieve low disease activity and decreased morbidity and mortality. To address these educational needs, we implemented a multimodal educational initiative supported by an independent medical educational grant. The content focused on equipping clinicians with knowledge and practical strategies to close clinical gaps, improve outcomes, and reduce disparities for patients with SLE and LN.
Methods: Three 1-hour, CE/CME-certified live webinars were delivered between April and May 2022. The webinars featured 2 expert faculty—1 rheumatologist and 1 nephrologist—and discussed strategies for SLE diagnosis, LN screening, incorporating novel therapies, and addressing disparities in practice, followed by a live question and answer session. Of note, 27% of the program content focused on disparities, including 7 practical ways clinicians can address disparities in practice. An online enduring recorded webcast was launched to extend the reach of the education to learners who could not attend the live webinars. Finally, 2 expert interview podcasts were developed to reinforce key takeaways from the program. Learner demographics were captured and summarized using descriptive statistics. Knowledge and competence were captured through pre- and post-activity questions and analyzed using a Chi square analysis.
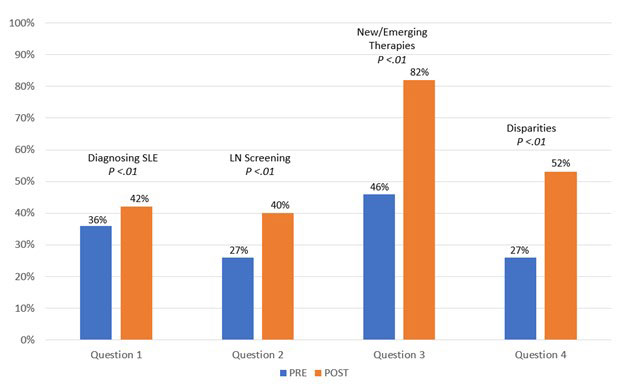
Results: To date, 361 learners have participated in the program, with interprofessional representation: physicians (47%, including rheumatologists [16%]), pharmacists (20%), NPs/PAs (19%), and RNs (6%). Learners have reported that nearly 1000 patients are likely to benefit because of this educational program. Preliminary pre- vs post-activity knowledge and competence improved across the domains as follows: diagnosing SLE (36% vs 42%; P = .5), screening for LN (26% vs 40%; P = .07), new/emerging therapies (46% vs 82%; P < .001), and healthcare disparities (26% vs 53%; P < .001).
Conclusion: These data support the use of a multimodal, multidisciplinary educational design strategy for improving and reinforcing learner knowledge and competence regarding diagnosis, treatment, and disparities in SLE and LN practice.2
References:
1. Ramos PS. Curr Opin Rheumatol. 2021;33:598-604.
2. Moore DE Jr, Green JS, Gallis HA. J Contin Educ Health Prof. 2009;29:1-5.
To cite this abstract in AMA style:
Handley L, Lovin Nealy K, Nisly S. Impact of Multimodal Independent Medical Education on Improving Outcomes and Reducing Disparities in Systemic Lupus Erythematosus and Lupus Nephritis [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/impact-of-multimodal-independent-medical-education-on-improving-outcomes-and-reducing-disparities-in-systemic-lupus-erythematosus-and-lupus-nephritis/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-multimodal-independent-medical-education-on-improving-outcomes-and-reducing-disparities-in-systemic-lupus-erythematosus-and-lupus-nephritis/