Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Serious infections are a major cause of morbidity and mortality in patients with RA, but less is known about more common, non-serious infections. We aimed to assess the frequency of common infections and their effect on medication interruptions, quality of life, and disease flares.
Methods: We remotely recruited adults with RA July 2022-July 2023 who reported current DMARD use and were patients within the Excellence Network in RheumatoloGY (ENRGY), a community rheumatology practice-based research network (PBRN). Participants joined the ArthritisPower Registry (now PatientSpot) using a smartphone or computer and completed a baseline survey and up to 6 monthly follow-up surveys, reporting current medications, presence and severity of flares in the past 30 days (1-10 scale), patient-reported outcomes (PROs) including Patient-Reported Outcomes Measurement Information System (PROMIS) measures and the Work Productivity and Activity Impairment General Health questionnaire (WPAI), infections in the past 30 days, and medication interruptions due to infection. Characteristics of infections and associations with medication interruptions were assessed. The impact of infections was evaluated by comparing PROs, productivity, and flares in those with vs. without an infection, using linear and logistic regression with generalized estimating equations to account for correlations within patients.
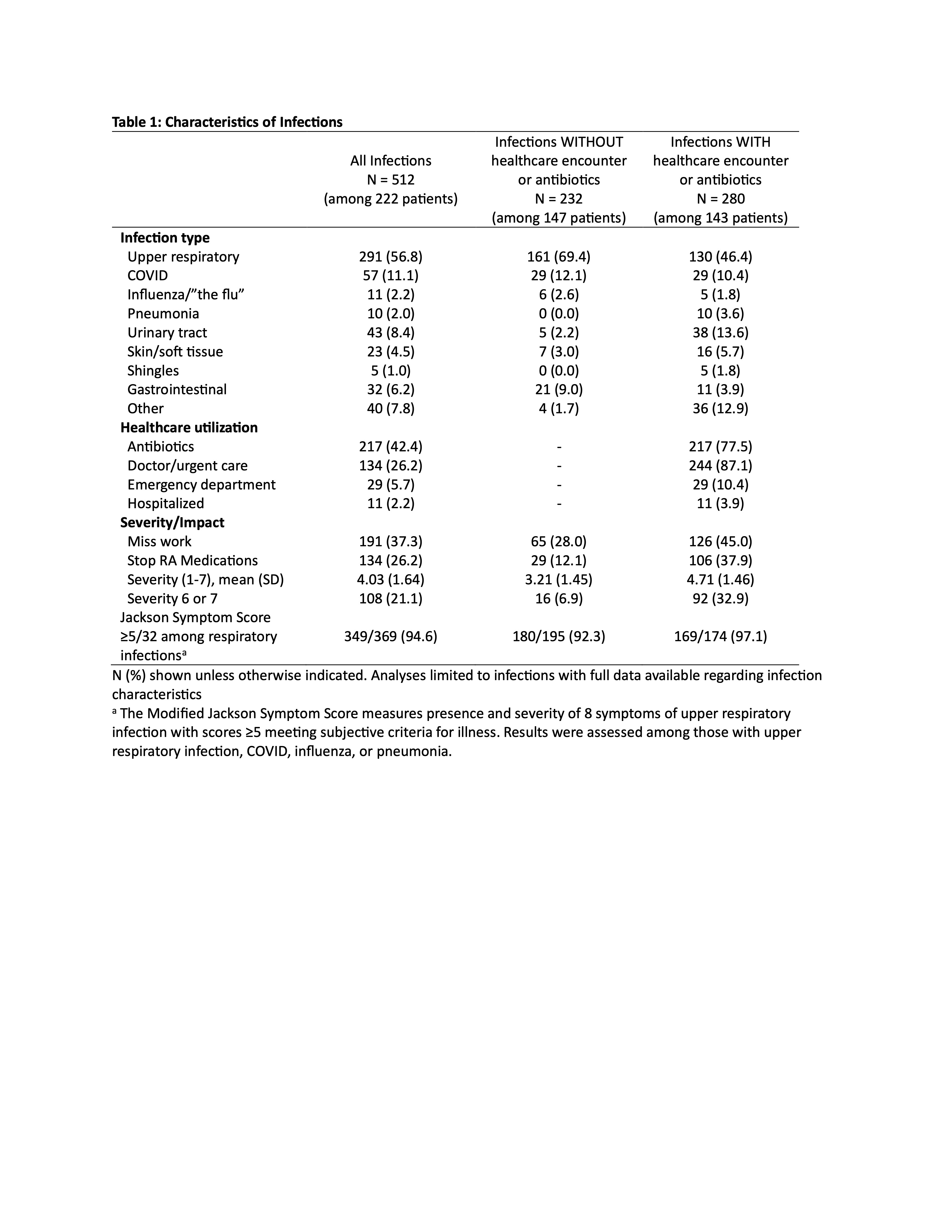
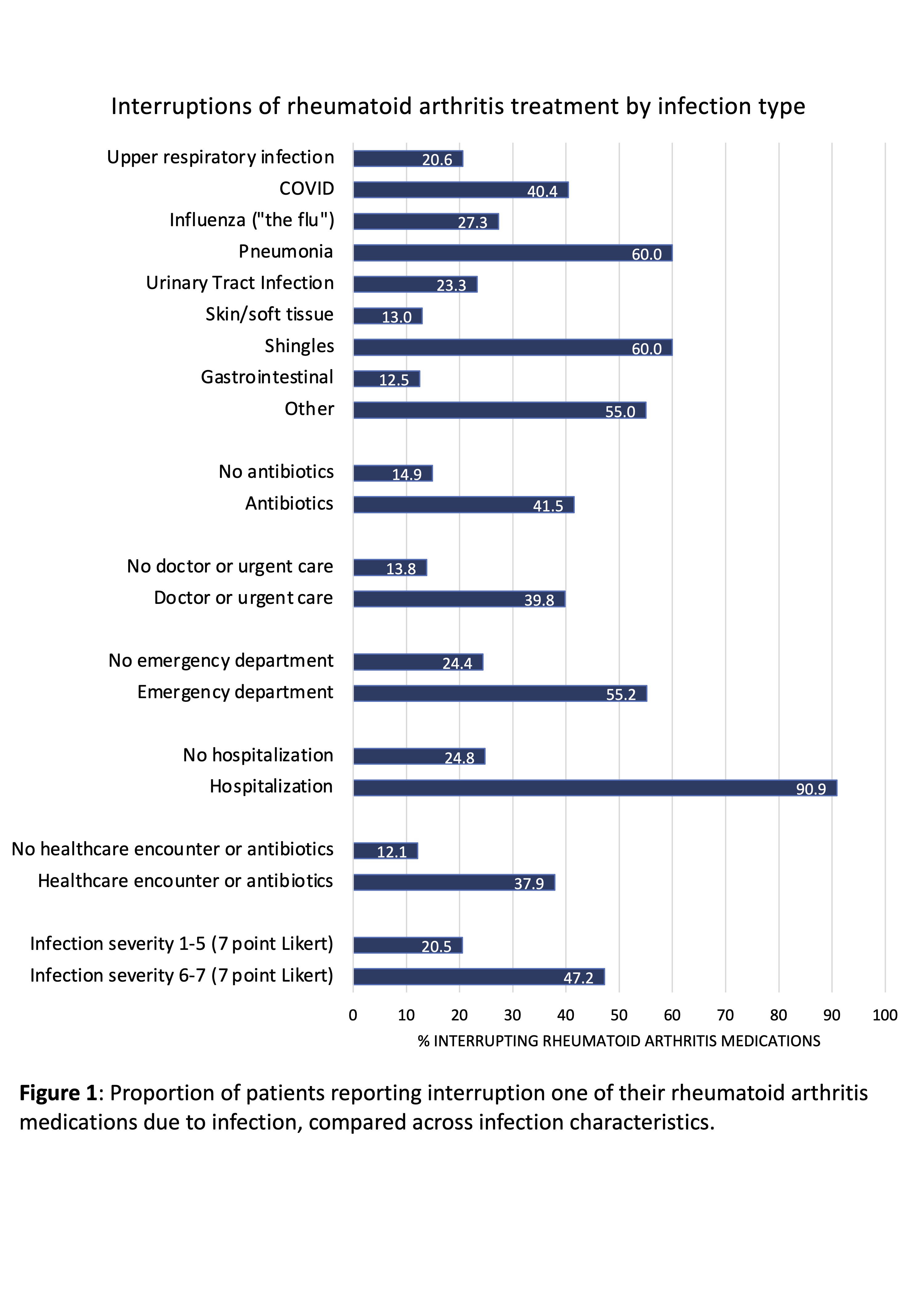
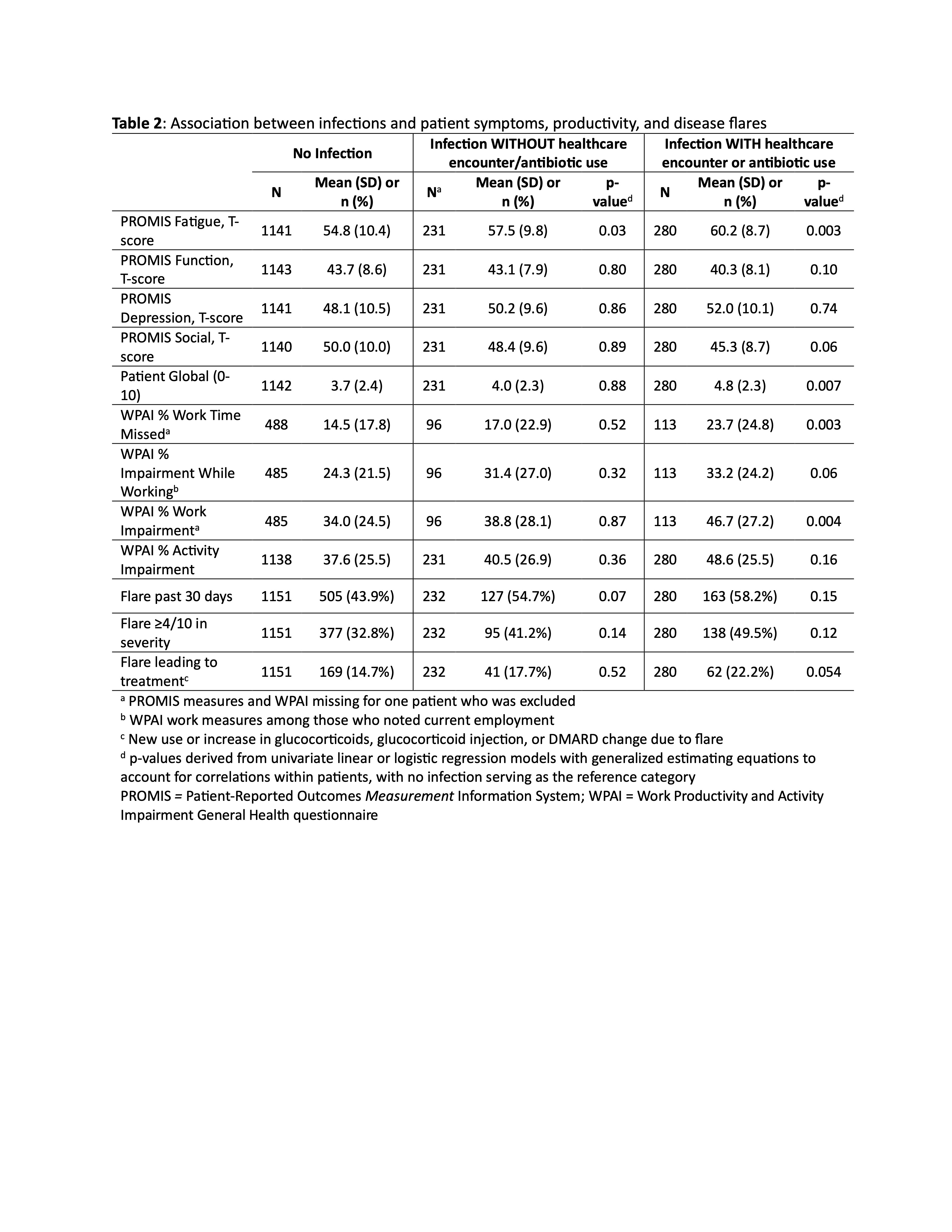
Results: We recruited 351 patients with RA (98% confirmed by EHR diagnosis) who contributed 1674 monthly observations (median 6, interquartile range 2-7). Patients had mean age of 60; 84% were female and 87% non-Hispanic White. At baseline, 78% were receiving a biologic or JAKi. A total of 523 infections (31% of observations) were reported by 224 unique patients, with infection details available for 512 infections (Table 1). Upper respiratory infections were the most frequent. Emergency department visits and hospitalizations for infection were uncommon, but 280 (55%) of infections led to a healthcare encounter or antibiotic use. Infections frequently led to missed work (37%) or interruptions in RA medications (27%). RA medication interruptions varied by infection type and were more common in those with vs. without healthcare encounters or antibiotic use (38% vs. 12%) and in infections rated 6-7 vs. 1-5 out of 7 in severity (47% vs. 20%) (Figure 1). Patients who experienced an infection had worse scores for PROMIS Fatigue but not PROMIS Function, Depression, or Social (Table 2). Differences were greater for infections leading to healthcare encounters or antibiotics, and these infections also were associated with worse Patient Global and more missed work and work impairment (Table 2). Frequency of disease flares was greater in those with vs. without infection, although differences were not statistically significant (Table 2).
Conclusion: Infections are common in patients with RA and frequently lead to medication interruptions. These infections also have an important impact on fatigue and work productivity and may lead to more disease flares. Clinicians should be aware of the effects of these infections on both RA treatment interruptions and patient symptoms.
To cite this abstract in AMA style:
George M, Gavigan K, Venkatachalam S, Curtis D, Stradford L, Nowell W, Baker J, Xie F, Curtis J. Impact of Common Infections on Medication Interruptions, Quality of Life, and Disease Flares in Patients with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/impact-of-common-infections-on-medication-interruptions-quality-of-life-and-disease-flares-in-patients-with-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-common-infections-on-medication-interruptions-quality-of-life-and-disease-flares-in-patients-with-rheumatoid-arthritis/