Session Information
Date: Tuesday, November 9, 2021
Title: Abstracts: Patient Outcomes, Preferences, & Attitudes (1909–1914)
Session Type: Abstract Session
Session Time: 2:00PM-2:15PM
Background/Purpose: Literature has shown poor adherence to antimalarial (AM) medications in rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE) patients, with the percentage of adherers ranging from 25% to 57%. However, the impact of AM adherence on cardiovascular (CVD) mortality has not been extensively studied. Our objective is to examine the association between AM adherence and CVD mortality among newly diagnosed incident RA and SLE patients.
Methods: We used administrative databases from British Columbia (BC), Canada, to conduct a retrospective study of population-based incident RA and SLE cohorts with incident AM use. The incident RA and SLE cases first met previously published RA, and SLE, criteria using administrative data between January 1997 and March 2015. Follow-up started on the first day of receiving AM and meeting either RA or SLE criteria. Subjects were followed until they died, left BC, or March 2015, whichever occurred first. The outcomes were mortality for the following CVD causes: myocardial infarction (MI), stroke, or venous thromboembolism (VTE). We used marginal structural models (MSM) to estimate the effect of AM adherence on CVD mortality, accounting for potential confounders and competing events due to death unrelated to CVD. In the analysis, follow-up time was divided into 90-days windows. For each window, the proportion of days covered (PDC), representing the proportion of time when medications were taken as prescribed, was calculated and categorized as adherent (PDC≥0.90), non-adherent (0< PDC< 0.90), and discontinued (PDC=0). The analyses were controlled for baseline demographics and the indicator of having RA or SLE, as well as the following sets of baseline and time-varying covariates: medication usage, health resource utilization, comorbidities, and Romano adaptation of Charlson comorbidity index (see footnote of Table 1). The MSM analysis produces valid estimates in the presence of time-varying confounding and competing events by balancing the distributions of time-varying confounders among the three adherence groups through inverse probability weighting.
Results: We identified 21,114 individuals with incident RA or SLE (mean age 55.8 years, 75.9% were women) who had filled at least one AM prescription. Over the mean follow-up of 8.6 years, 900 (4.3%) patients died due to a CVD cause: MI, stroke, or VTE. The incidence rate (IR) of CVD mortality when patients were adherent, non-adherent, and discontinued AM were 3.10, 4.68, and 5.65 per 1000 person-years. Using MSM, the adjusted CVD mortality hazard ratios (HRs) obtained for AM non-adherence and adherence in RA or SLE patients were 1.08 (95% CI: 0.91-1.31) and 0.51 (95% CI: 0.42-0.62), respectively, relative to discontinuation (Table 1). Also, the adjusted HR for adherence compared to non-adherence was 0.47 (95% CI: 0.37-0.60). Similar findings were obtained for each cause of CVD mortality individually except VTE (Table 2).
Conclusion: When RA and SLE patients adhere to AM therapy, they have a 49% lower risk of CVD mortality than when patients discontinue AM. Also, the protective effect of AM was not observed when patients were taking less than 90% of the prescribed AM dose.
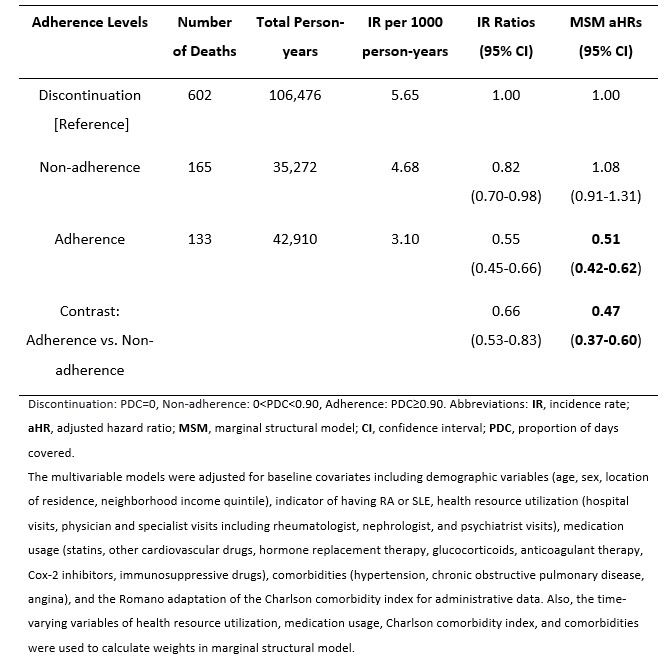 Table 1. Overall risk of CVD mortality in incident RA and SLE patients during follow-up
Table 1. Overall risk of CVD mortality in incident RA and SLE patients during follow-up
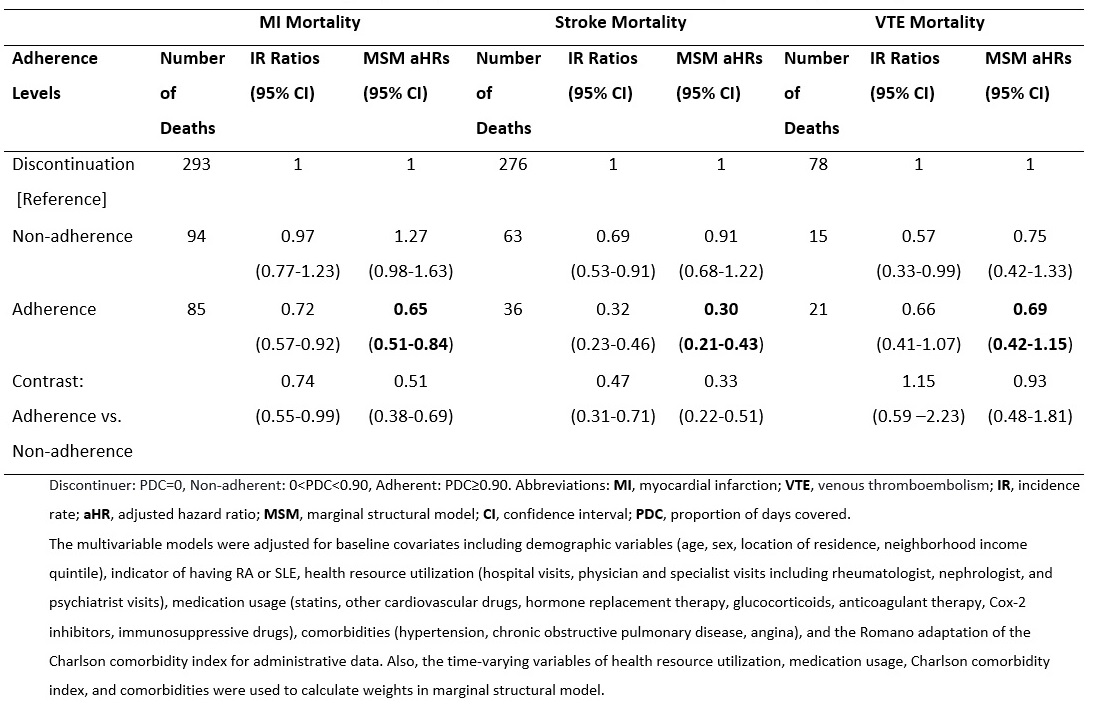 Table 2. Overall risk of death caused by MI, stroke, and VTE in incident RA and SLE patients during follow-up
Table 2. Overall risk of death caused by MI, stroke, and VTE in incident RA and SLE patients during follow-up
To cite this abstract in AMA style:
Hoque M, Avina-Zubieta J, Lacaille D, De Vera M, Qian Y, Esdaile J, Xie H. Impact of Antimalarial Adherence on Cardiovascular Mortality Among Patients with Newly Diagnosed Rheumatoid Arthritis and Systemic Lupus Erythematosus: A Population-based Study [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/impact-of-antimalarial-adherence-on-cardiovascular-mortality-among-patients-with-newly-diagnosed-rheumatoid-arthritis-and-systemic-lupus-erythematosus-a-population-based-study/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-antimalarial-adherence-on-cardiovascular-mortality-among-patients-with-newly-diagnosed-rheumatoid-arthritis-and-systemic-lupus-erythematosus-a-population-based-study/
