Session Information
Date: Sunday, November 13, 2022
Title: SLE – Diagnosis, Manifestations, and Outcomes Poster II: Manifestations
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
Background/Purpose: The aim of this study is to assess the incidence of Systemic Lupus Erythematosus (SLE) in a cohort of patients with Immune Thrombocytopenic Purpura (ITP), and to identify predictors for its development.
Methods: Retrospective cohort study. We included all patients with ITP treated in a University Hospital between 2000 and 2018, with at least one year of follow-up. Patients with SLE or other secondary causes of ITP were excluded. Demographic, clinical, laboratory and treatment data were recorded at diagnosis of ITP and at the end of follow-up. Patients meeting SLE classification criteria (ACR 1997 / SLICC 2012) during the follow-up were identified, and the density incidence of SLE was calculated. Patients with ITP were grouped according to the development or non-development of SLE, and comparisons between groups were made. Univariate analysis was performed to identify factors associated with the future development of SLE.
Results: 186 patients were included, 64.5% (95%) women, with a median age of 27.2 years (IQR 6.3-63.9). After a follow-up of 1801.4 person/years (py), 10 patients (5.4%) developed SLE, with a median time of 22.9 months (IQR 9.8-60.9) between ITP diagnosis and development of SLE. The incidence density of SLE was 5.6/1000 py (95% CI 2.9-9.9/1000 py). The characteristics of both groups are shown in Table 1.
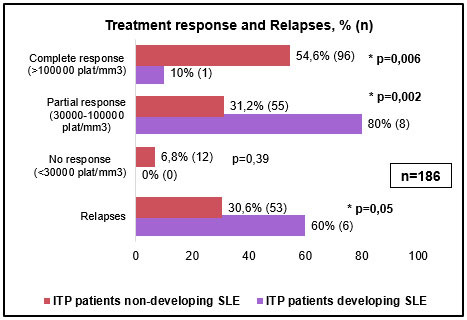
At diagnosis of ITP, only 31 patients (16.7%) were assessed by a rheumatologist. Patients who developed SLE had significantly higher proportion of chronic ITP (80% vs 40.3%; p=0.01), lower proportion of complete response (10% vs 54.6%; p=0.006), and more relapses (60% vs 30.6%; p=0.05). The median duration of ITP in patients with SLE was significantly longer (67.5 vs 4 months, p< 0.001).
The presence of positive ANA (p< 0.001), nuclear homogeneous pattern (p< 0.001), ANA titres ≥1/640 (p=0.02), hypocomplementemia (p< 0.001), lupus anticoagulant (p< 0.001), polyclonal hypergammaglobulinemia (p< 0.001), leukopenia (p=0.006) and hemolytic anemia (p=0.005) were significantly associated with the future development of SLE.
Conclusion: In this cohort of patients with ITP, the incidence density of SLE was 5.6/1000 py. The most refractory course of the disease, as well as the presence of homogeneous pattern and high titre ANA, hypocomplementemia, lupus anticoagulant, polyclonal hypergammaglobulinemia and other cytopenias were significantly associated with the subsequent development of SLE.
To cite this abstract in AMA style:
Alle G, Scolnik M, SCAGLIONI V, Jaramillo Gallego J, Tobar Jaramillo M, Alvarado R, Soriano E, Rosa J. Immune Thrombocytopenic Purpura and Subsequent Development of Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/immune-thrombocytopenic-purpura-and-subsequent-development-of-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/immune-thrombocytopenic-purpura-and-subsequent-development-of-systemic-lupus-erythematosus/