Session Information
Date: Monday, October 27, 2025
Title: (1088–1122) Immunological Complications of Medical Therapy Poster
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Patients (pts) with rheumatoid arthritis (RA) face a higher lifetime burden of cardiovascular disease (CVD) vs the general population with approximately 1.5-2-fold increase in heart failure, myocardial infarction and CVD mortality. Recent data suggest that immune checkpoint inhibitors (ICIs), a major anti-cancer therapy class, may also contribute to CVD risk. We conducted a comparative evaluation of CVD outcomes in pts with cancer receiving ICI-based therapy, focusing on differences between those with vs without pre-existing RA. We hypothesized that pts with pre-existing RA receiving ICI-based therapy would have a higher risk of adverse CVD events vs those without RA.
Methods: We conducted a population-based cohort study using electronic health records of pts with cancer receiving ICIs between 2011 and 2025 from 101 U.S. healthcare organizations. We identified pts with pre-existing RA using at least two diagnostic codes who were treated with anti-programmed death-1/programmed death ligand-1 (PD-1/PD-L1) and/or cytotoxic T-lymphocyte associated protein 4 (CTLA4) agents. We calculated propensity scores using covariates including demographics (age, sex, race/ethnicity), comorbidities, cancer type, metastatic status, previous and concurrent anti-cancer treatments, history of exposure to statins and systemic steroids. Pts with RA on ICI were propensity-score matched 1:1 with pts treated with ICI without RA. We used Cox proportional hazards models to assess the risk of individual outcomes of all-cause mortality, stroke, ischemic heart disease, including myocardial infarction and heart failure.
Results: We analyzed 2,270 pts with pre-existing RA treated with ICI and 2,270 propensity score-matched comparators (Table 1). Mean age was 69 years, 60% were female, 78% were White. After initiation of ICI-based therapy, over a mean follow-up of 47.6 months, pts with RA did not have a significantly higher risk of all-cause mortality (HR 1.03, 95% CI 0.94–1.12) or stroke (HR 0.99, 95% CI 0.86–1.14) vs pts without RA. However, the risk for ischemic heart disease (HR 1.35, 95% CI 1.13–1.62), specifically myocardial infarction (HR 1.49, 95% CI 1.16–1.91) and heart failure (HR 1.25, 95% CI 1.02–1.54) were higher for pts with RA vs pts without RA (Figure 1).
Conclusion: Among pts on ICI-based therapy, those with pre-existing RA did not have significant higher all-cause mortality or risk for stroke, but higher risk of ischemic heart disease and heart failure vs pts without RA. Our hypothesis-generating findings are consistent with the known CVD burden in pts with RA and cancer that may be possibly exacerbated by ICI. Further studies are needed to validate our data and, also, investigate prophylaxis, early diagnosis and proper management of CVD in pts with RA receiving ICI-based therapy for cancer.
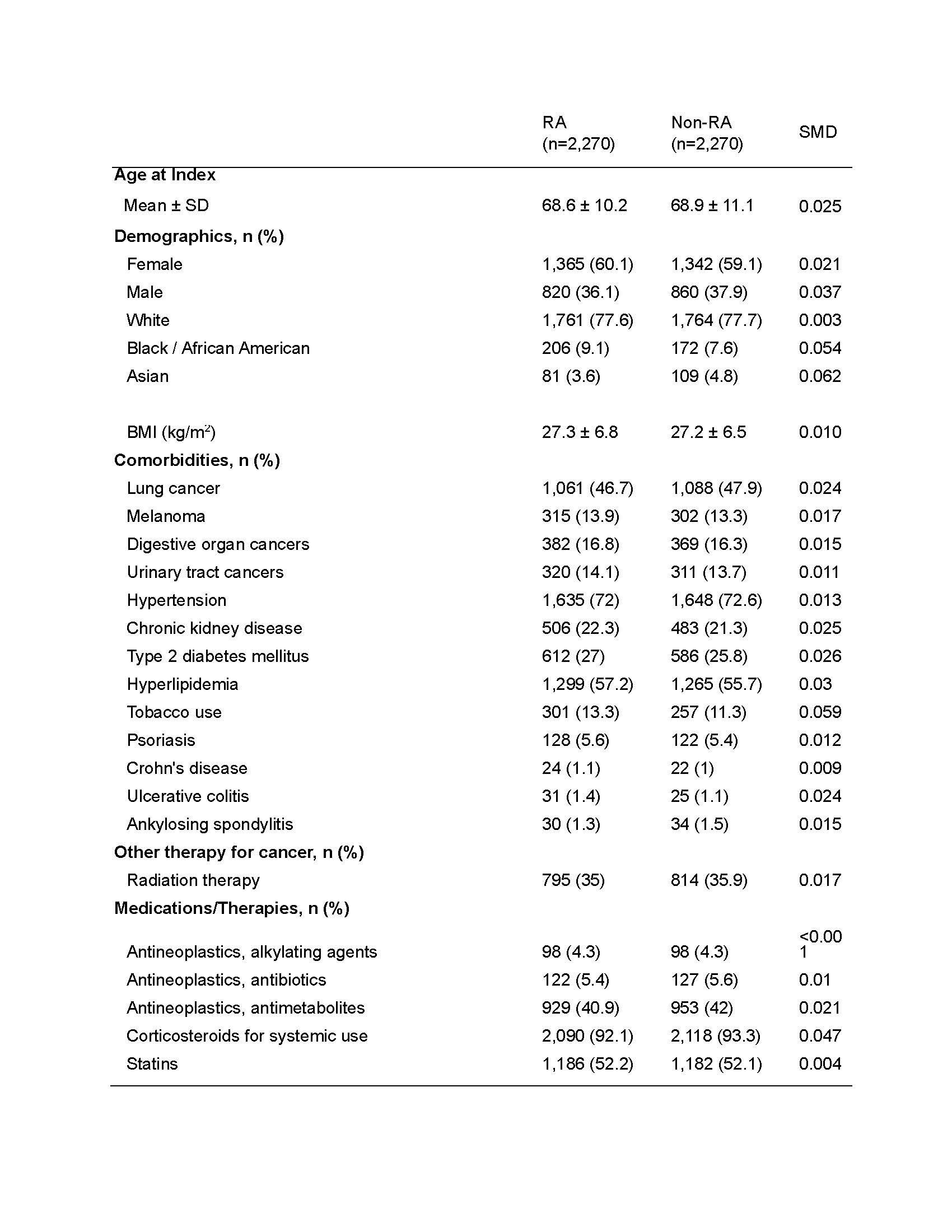 Table 1. Baseline characteristics of pts on ICI with and without pre-existing RA, after propensity score matching
Table 1. Baseline characteristics of pts on ICI with and without pre-existing RA, after propensity score matching
.jpg) Figure 1. Risk of cardiovascular outcomes in persons with cancer on ICI with versus without RA
Figure 1. Risk of cardiovascular outcomes in persons with cancer on ICI with versus without RA
To cite this abstract in AMA style:
Sheng-Kai Ma K, Stovall R, Sparks J, Wu Y, Cheng R, Challener G, von Eckstaedt H, Bansal B, Grivas P, Chen S, Liew J, Singh N. Immune Checkpoint Inhibitors and Cardiovascular Risk in Patients with Rheumatoid Arthritis and Cancer [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/immune-checkpoint-inhibitors-and-cardiovascular-risk-in-patients-with-rheumatoid-arthritis-and-cancer/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/immune-checkpoint-inhibitors-and-cardiovascular-risk-in-patients-with-rheumatoid-arthritis-and-cancer/
