Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Antiphospholipid syndrome (APS) is an autoimmune coagulopathy that causes microvascular and macrovascular thrombosis in both venous and arterial systems. This can occur as a primary autoimmune disease or secondary with other autoimmune disease, most commonly SLE. The current 2023 ACR/EULAR APS classification requires a thrombotic event with the serological presence of a lupus anticoagulant, anti-cardiolipin antibodies (ACLA) or anti-B2 glycoprotein I antibodies (β2GPI) detected on two separate occasions at least 12 weeks apart. Recently, “non-criteria” antibodies have gained attention as potential risk for APS. Here, we investigated the utility of anti-phosphatidylserine (PS) antibodies in patients with established diagnosis of APS with or without SLE with a goal to improve classification and diagnostic accuracy and promote timely intervention.
Methods: This was a retrospective analysis of electronic medical records of patients tested in the laboratory of SUNY Upstate University Hospital between 2012 and 2024. We analyzed a total of 1286 patients tested for the presence of IgA, IgG, and IgM PS antibodies. We also evaluated the utility of IgA, IgM, and IgG β2GPI and ACLA and lupus anticoagulant assays: hexagonal phase phospholipid (HPPNA), diluted Russell viper venom time (DRVVT), and platelet neutralization procedures (PNP). This12-component panel has been established for screening for aPL reactivity at our institution. For statistical analyses, we employed chi-square, Fisher’s exact test and Bonferroni correction for multiple comparison using the GraphPad V10.
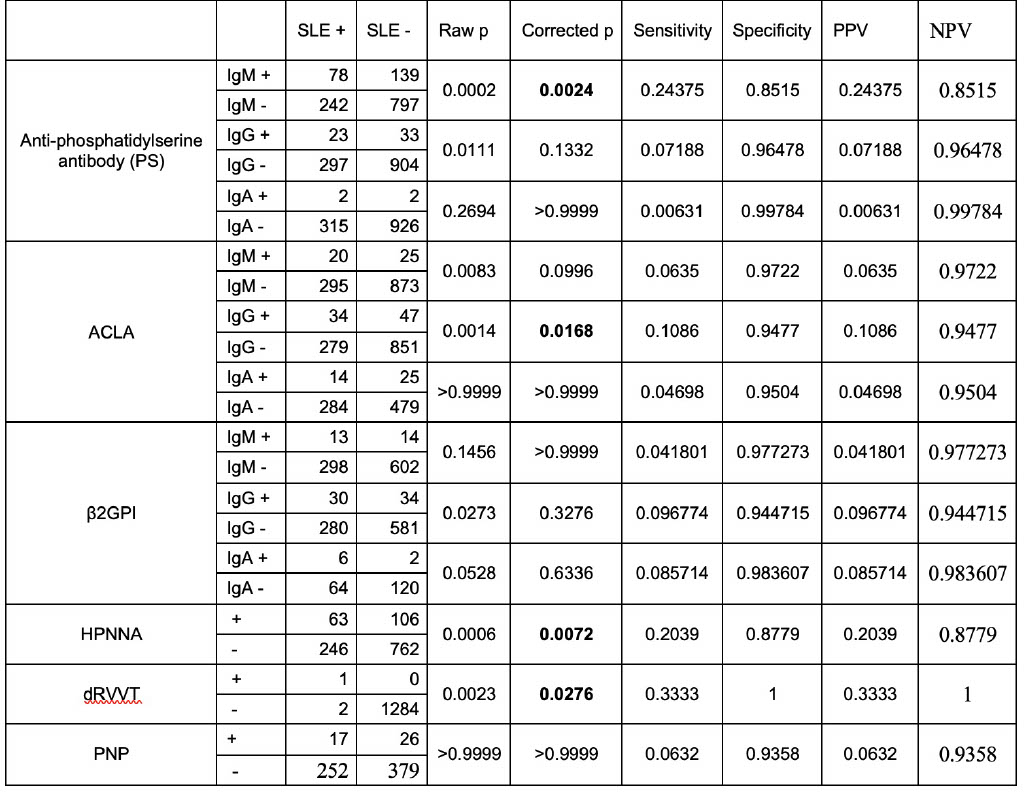
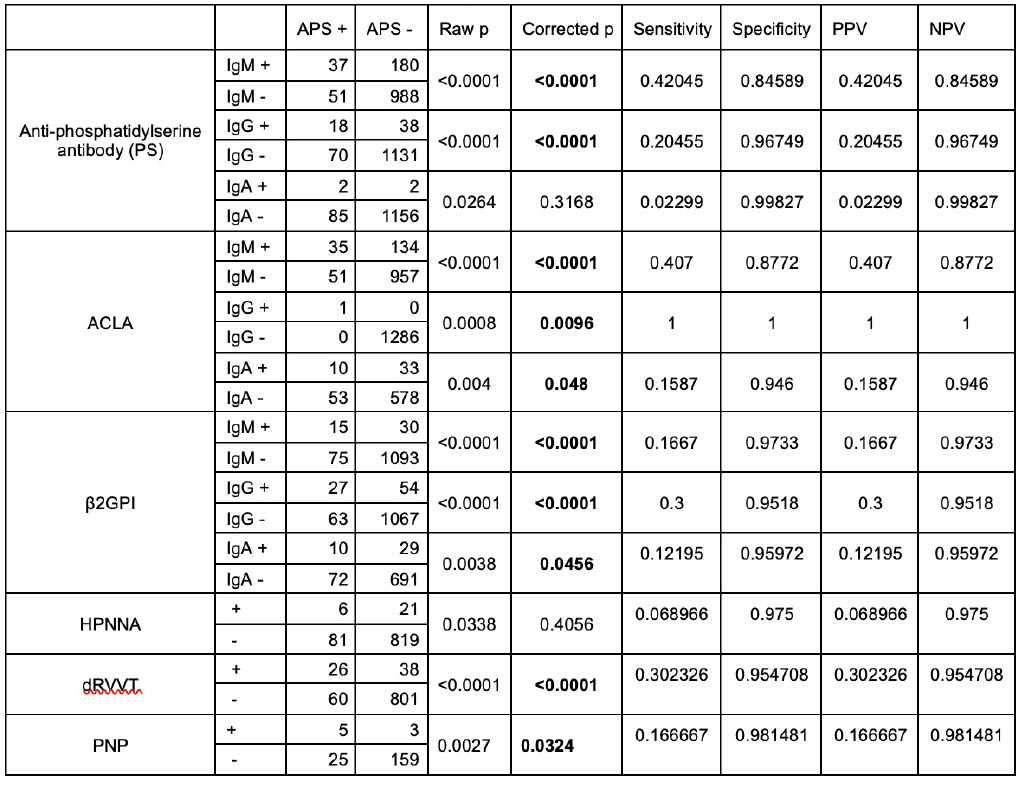
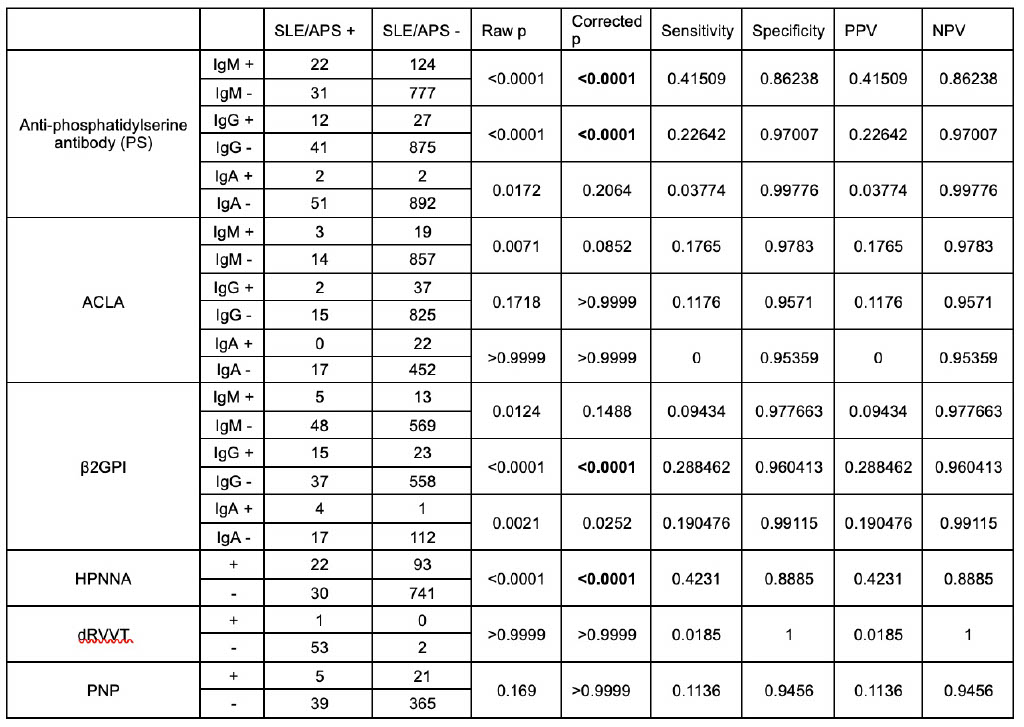
Results: There was a total of 322 SLE patients (Table 1), 90 APS patients (Table 2), and 54 patients with concurrent SLE and APS who undergone simultaneous testing for IgA, IgG, and IgM PS, ACLA, and β2GPI antibodies and HPPNA, DRVVT, and PNP assays (Table 3). Our results indicate that IgM PS antibody is most useful for discriminating patients with SLE (Table 1, p=0.0024), APS (Table 2, p< 0.0001), and SLE/APS from those not having either of these diagnosis (Table 3, p< 0.0001). IgG PS antibody is useful for discriminating patients with APS (Table 2, p< 0.0001) and SLE/APS from those not having either of these diagnosis (Table 3, p< 0.0001). Amongst 322 patients with SLE, 31 patients only had a positive IgM PS antibody, 8 different patients only had a positive IgG PS antibody, while none had IgA PS antibody.
Conclusion: These results demonstrate a significant utility of IgM and IgG PS antibody testing for the workup of patients with SLE and APS. Detection of IgM and IgG PS antibody may allow for more precise classification, sensitive diagnosis, and timely treatment of patients with relevant clinical manifestations. Further research aimed at the inclusion of these antibodies in laboratory classification criteria of SLE and APS is strongly warranted.
To cite this abstract in AMA style:
Donath C, Kahlown S, Soares R, Gautam K, Saleh M, Katalin B, Perl A. IgM and IgG Phosphatidylserine Antibody Detection May Improve Classification Accuracy of SLE and APS [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/igm-and-igg-phosphatidylserine-antibody-detection-may-improve-classification-accuracy-of-sle-and-aps/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/igm-and-igg-phosphatidylserine-antibody-detection-may-improve-classification-accuracy-of-sle-and-aps/