Session Information
Session Type: Abstract Session
Session Time: 2:00PM-3:30PM
Background/Purpose: COPA syndrome is a rare, severe monogenic autoinflammatory/autoimmune disorder with variable penetrance, most commonly affecting the lungs and joints. It is caused by dominant negative mutations located in a specific hot spot (from the 7th to the 10th exons) of the COPA gene on chromosome 1, encoding the α subunit of the COP1 complex involved in protein transport from the Golgi apparatus to the endoplasmic reticulum. COPA syndrome is associated with autoimmunity and upregulation of both the type 1 interferon pathway and T helper-17 cells. Clinical manifestations usually start during childhood, but late-onset diseases have been described with up to 30% of asymptomatic carriers. We aimed to identify additional novel non-synonymous variants (NSV) in COPA and to describe their associated phenotypes.
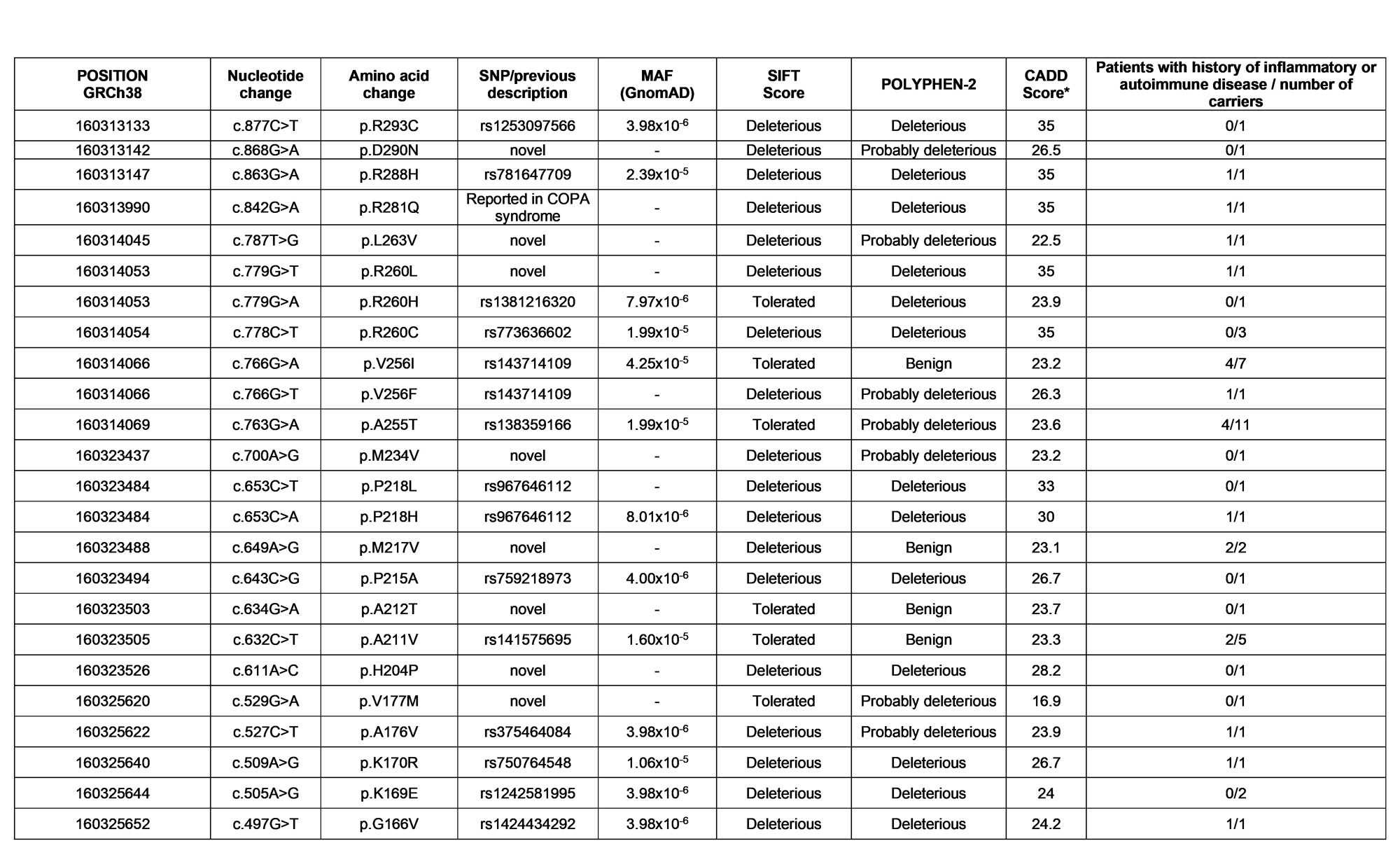
Methods: All individuals from a large institutional biobank of adults with available whole-exome sequencing (WES) data were included in this study. All NSV from the 7th to the 10th exons of COPA were identified and annotated according to allele frequency reported in an online database (gnomAD) and functional predictive tools (SIFT, POLYPHEN-2, and CADD score). Medical record review was performed for all NSV-carrying individuals to collect personal and family medical history as well as results of autoantibody testing and chest imaging obtained through routine clinical care.
Results: Among the 53,364 adults with available WES data, 24 unique NSV in the COPA hot spot were identified in a total of 48 individuals (prevalence 0.09%, Table 1); 33 were women (69%), median age at medical record review was 51.7 years (IQR 39.6, 64.5). Only one NSV (p.R281Q) had been previously reported as a mutation in a COPA syndrome. This patient developed seronegative RA at age 18 and autoimmune hepatitis at age 35 without clinically diagnosed COPA syndrome. All other identified NSV were novel to COPA syndrome: 15 with a frequency < 0.0001 and 8 never previously identified so unable to estimate known frequency. Deleterious impact was predicted by both SIFT and POLYPHEN-2 for 12 variants (50%). Autoimmune or inflammatory disease was reported for 21 of the 48 carriers (44%); median age at disease onset was 42.9 years (IQR 28.2, 56.0; Table 2). 19/21 (91%) had adult-onset of these diseases. Inflammatory arthritis occurred in 6 patients, 4 diagnosed as rheumatoid arthritis (RA). Interstitial lung disease was observed in 5 patients. Five patients had psoriasis and/or Crohn’s disease. Antinuclear antibodies, anti-CCP, and rheumatoid factor were positive for 9/15, 3/8 and 4/9 patients, respectively. A family history of autoimmune/inflammatory disease was reported in 9 patients. Two individuals died, both from acute on chronic heart failure, at ages 64 and 79.
Conclusion: In this first investigation of COPA in a large adult biobank, we identified 23 novel NSV beyond the known causal mutations and described associations with inflammatory and autoimmune diseases among nearly half of SNV, most of which were adult-onset. If functional impact of the newly identified NSV is proven, rare exonic NSV in COPA could contribute to the genetic architecture of several common autoimmune and inflammatory phenotypes.
To cite this abstract in AMA style:
Juge P, McDermott G, Hayashi K, Cui J, David-Gabarre C, Frémond M, Wobma H, Raychaudhuri S, Karlson E, Dieudé P, Sparks J. Identification of 23 Novel COPA Rare Exonic Non-Synonymous Variants and Their Associated Autoimmune and Inflammatory Clinical Phenotypes Among 53,364 Individuals [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/identification-of-23-novel-copa-rare-exonic-non-synonymous-variants-and-their-associated-autoimmune-and-inflammatory-clinical-phenotypes-among-53364-individuals/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/identification-of-23-novel-copa-rare-exonic-non-synonymous-variants-and-their-associated-autoimmune-and-inflammatory-clinical-phenotypes-among-53364-individuals/