Session Information
Session Type: Abstract Session
Session Time: 3:00PM-4:30PM
Background/Purpose: The prevalence of vitamin D deficiency is higher in patients with systemic lupus erythematosus (SLE) compared to the healthy population, and recent studies have observed a higher prevalence of hypovitaminosis D in patients with associated kidney disease. This deficiency has been proposed as a risk factor for a higher incidence and activity of autoimmune diseases. The present study aims to determine the prevalence of hypovitaminosis D and its correlation with clinical and renal activity and histopathological findings of renal biopsy in patients with SLE and lupus nephritis (LN).
Methods: Analytical cross-sectional study, in patients with SLE according to the 2019 EULAR/ACR criteria and lupus nephritis by renal biopsy according to ISN/RPS of 2003. A measurement of disease activity was performed by SLEDAI 2K considering high activity > 4 points, and renal activity through creatinine, BUN, urinary sediment, albuminuria, urinary creatinine protein ratio, 24-hour urine protein count, GFR, renal biopsy report, activity index and chronicity. Serum vitamin D levels were measured by ELISA (Human soluble 25-OH Vitamin D ELISA Kit Eagle Bioscences), considering hypovitaminosis D < 30 ng/mL. The sample calculation was carried out with the formula for difference of proportions with a statistical power of 85% requiring 24 patients. Quantitative variables were tested for Shapiro-Wilk normality and expressed as means and standard deviations. Qualitative variables were reported as frequencies and percentages. In the inferential analysis, the continuous variable of vitamin D levels was analyzed with the Student’s T test. Categorical variables were analyzed with the Chi2 test or Fisher’s exact test. The correlation analysis was performed using Pearson’s coefficient and Kendall’s Tau b for continuous and ordinal variables respectively. In all cases, bilateral statistics were performed with an alpha value < 0.05. SPSS v21 software was used for data analysis and Graph Pad Prism software was used to create graphs.
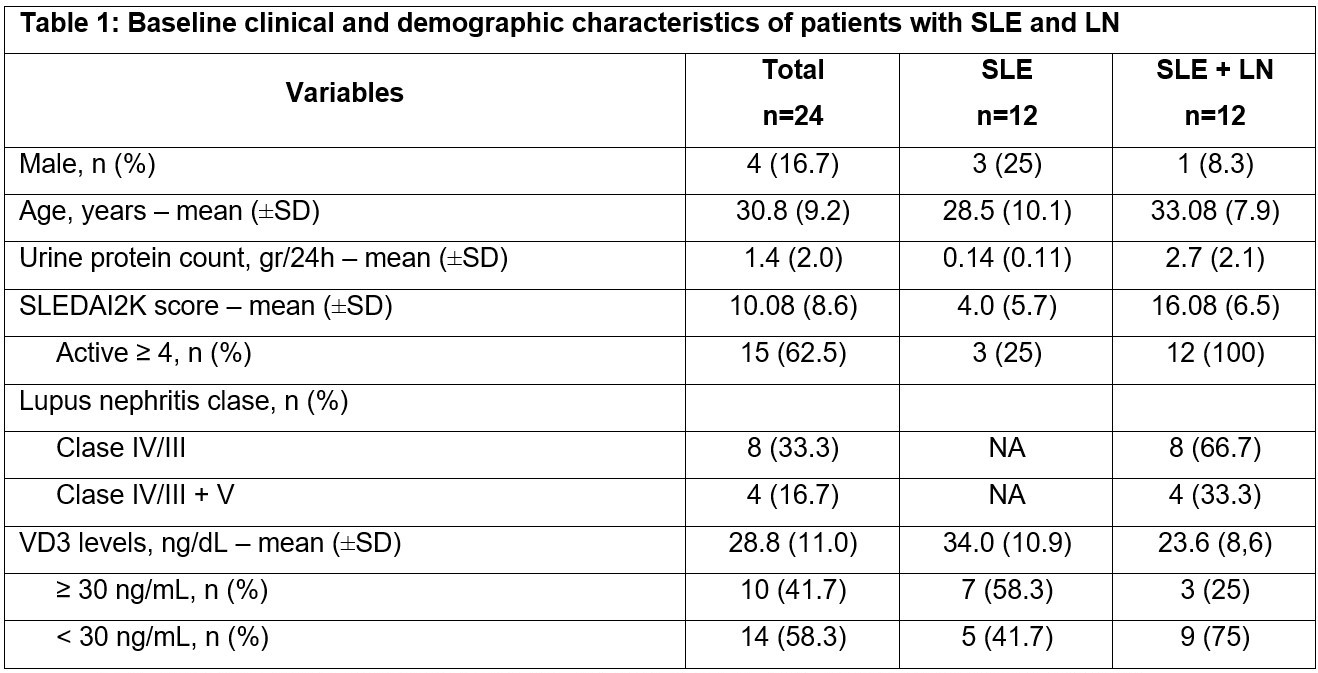
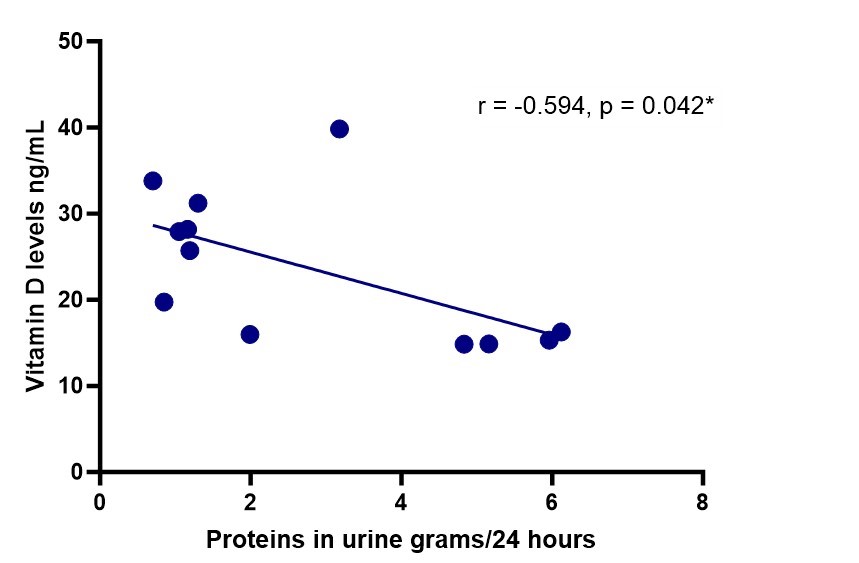
Results: Twenty-four patients with systemic lupus erythematosus were studied, divided into two groups: the first included 12 patients without renal involvement and the second included 12 patients with LN. 58% of the 24 patients had hypovitaminosis D, of which there was a higher prevalence in patients with LN than in the SLE group without kidney disease, 75% vs 42% (Table 1). Vitamin D level had a moderate negative correlation (Figure 1) with 24-hour urine protein count (r =-0.594, p=0.042) in patients with LN. In the renal biopsy lesions, 100% had rupture of the glomerular basement membrane (GBM) and interstitial inflammation, followed by endocapillary hypercellularity in 91.7%, but none was specifically correlated to hypovitaminosis D.
Conclusion: Hypovitaminosis D has a higher prevalence in patients with lupus nephritis compared to patients with SLE without kidney disease. In patients with lupus nephritis, the greater the proteinuria, the greater the vitamin D deficiency.
To cite this abstract in AMA style:
Yupe A, Puron Gonzalez E, Salatino E, Santana J, Ochoa M, Cervantes-Ramirez R, Saldaña E, Calderon g, Ceniceros B, de la Cruz U, Meza M, Cerpa Cruz S. Hypovitaminosis D in Lupus Nephitis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/hypovitaminosis-d-in-lupus-nephitis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/hypovitaminosis-d-in-lupus-nephitis/