Session Information
Date: Saturday, November 16, 2024
Title: SLE – Treatment Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Hydroxychloroquine (HCQ) is the cornerstone in treatment of systemic lupus erythematosus (SLE), yet its role in preventing kidney function decline in lupus nephritis (LN) is debated. While studies showed that HCQ prevents kidney damage in SLE and LN flares, Pokroy-Shapira et al. and Wu et al. reported worsening or no significant improvement in kidney function in LN with HCQ use. Given conflicting information, universal use of HCQ in LN could be limited despite guideline recommendations. Therefore, we analyzed data from our longitudinal inception cohort to examine the time-varying effect of HCQ on kidney function decline in LN.
Methods: Data were abstracted from adult LN patients who underwent kidney biopsy between 1994-2022 to confirm LN diagnosis. Data included demographics, social factors, comorbidities, and pathologic findings (LN class, chronicity & activity indices, renal arteriosclerosis) at LN diagnosis. All glomerular filtration rate (eGFR) values from 6 months before LN diagnosis through last follow-up were abstracted. Prescription data were abstracted to estimate HCQ exposure time after LN diagnosis. The primary outcome was sustained eGFR decline, defined as 30% or more reduction from baseline at the last 3 consecutive visits. We examined the association between HCQ exposure and the time to sustained eGFR decline using multivariable Cox regression models. We also calculated the eGFR slope to examine the time-varying effect of HCQ use on eGFR slope over time.
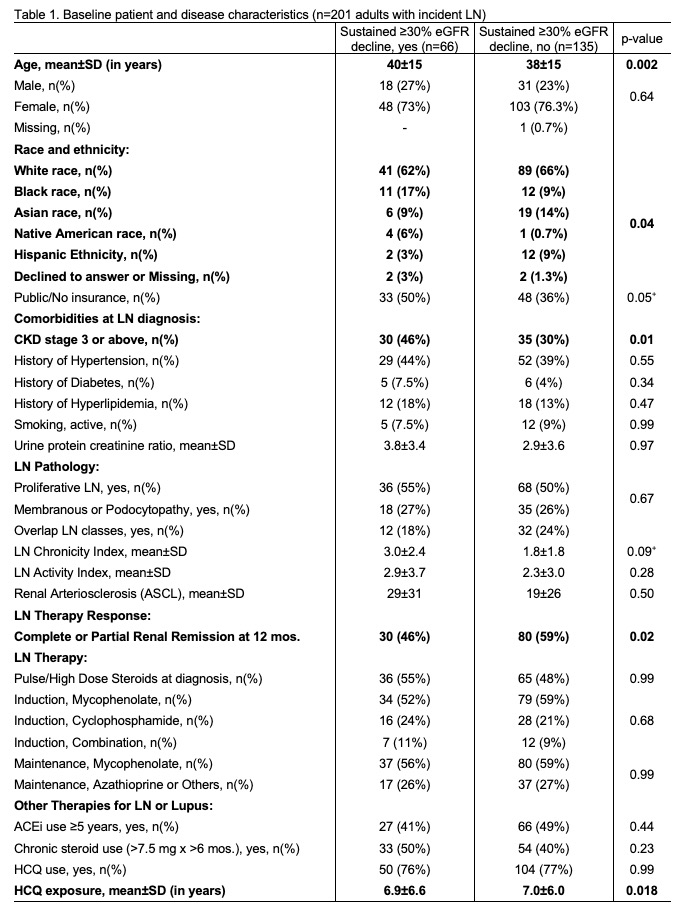
Results: Sixty six (33%) of 201 patients experienced a sustained eGFR decline (Table 1). Patients with sustained eGFR decline were older, more likely to have CKD stage ≥3 at diagnosis, and had shorter HCQ exposure time.
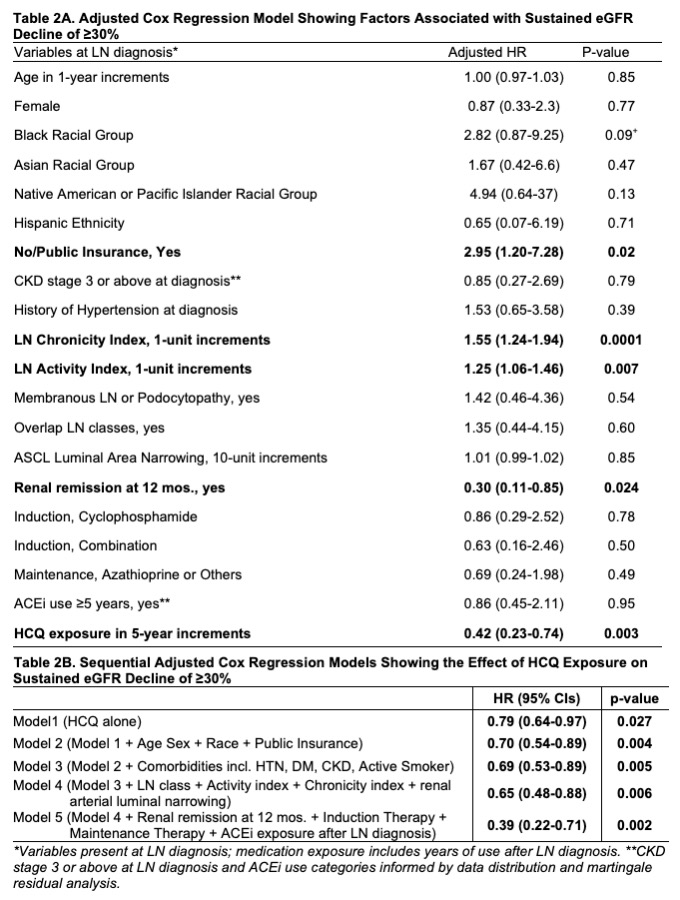
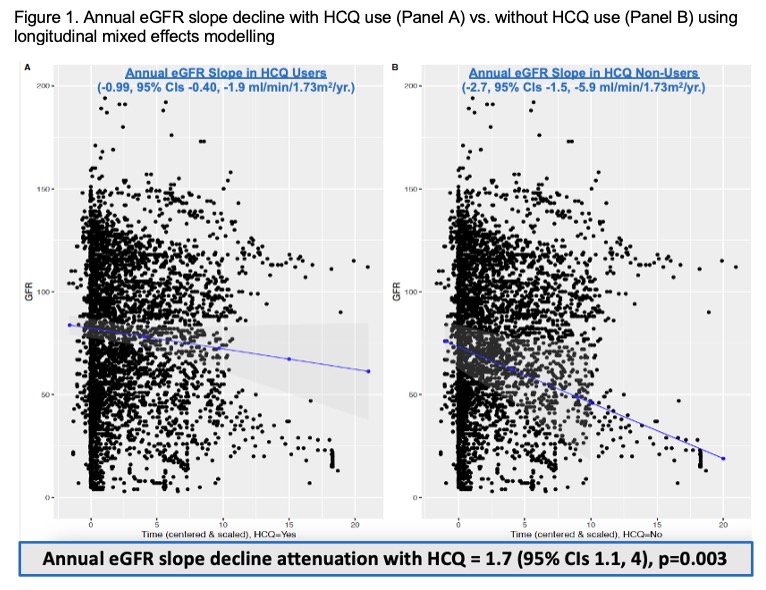
After adjusting for covariables, each 5-year increase in HCQ exposure was associated with 58% lower risk of sustained eGFR decline (adjusted HR (aHR) = 0.42, 95% CIs 0.23-0.74, p = 0.003; Table 2A). Chronicity & activity index scores and no/public insurance at LN diagnosis were associated with higher risk of eGFR decline, while achieving renal remission at 12 months was associated with a 70% lower risk of eGFR decline (Table 2A). HCQ exposure remained strongly associated with lower eGFR decline after adjusting for covariables and confounders (Table 2B). In a subgroup analysis including patients with CKD stage ≥3 at LN diagnosis, HCQ exposure was associated with 90% lower risk of eGFR decline (aHR 0.10, 95% CIs 0.03-0.40, p-value = 0.001, data not shown). Finally, eGFR slope differed significantly for HCQ users vs. non-users (Figure 1, -0.90 vs. -2.7 ml/min/1.73 m2/year; p=0.003).
Conclusion: In LN, HCQ use is significantly associated with a) 58% lower risk of sustained kidney function decline; b) 90% lower risk of kidney function decline in particularly those with chronic kidney disease stage 3 or more at lupus nephritis diagnosis; c) less steep eGFR slope over time. Future CKD prevention efforts should encourage HCQ use in all patients with LN and prospectively examine its impact on health outcomes in LN.
To cite this abstract in AMA style:
Garg S, Rovin B, Astor B, Singh T, Kolton L, Saric C, Lim S, Bartels C. Hydroxychloroquine Users at Lower Risk of Kidney Function Decline in Lupus Nephritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/hydroxychloroquine-users-at-lower-risk-of-kidney-function-decline-in-lupus-nephritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/hydroxychloroquine-users-at-lower-risk-of-kidney-function-decline-in-lupus-nephritis/