Session Information
Date: Saturday, November 7, 2020
Title: SLE – Treatment Poster I
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Hydroxychloroquine (HCQ) has been used for decades to treat systemic lupus erythematosus (SLE) and is associated with decreased lupus flares and damage. However, despite reports of an impact on TLR pathways, its mechanism of action remains controversial.
Methods: Whole blood from healthy controls (n=8) and SLE patients taking (n=9) or not taking HCQ (n=9) were stimulated for 15 minutes or 24 hours with either Toll-like receptor (TLR) (for TLR4, TLR7/8 or TLR9), interferon-α (IFNα), T cell (phytohemagglutinin and ionomycin), or cell signaling inducers (phorbol myristate acetate and ionomycin). Cell culture supernatants and phospho-proteins were analyzed. Cytokine levels from patient plasma and culture supernatants were assessed by 37-plex xMAP assays and ELISAs. Alterations in phospho-signaling proteins were assessed by mass cytometry. To determine alterations in phospho-signaling pathways, whole blood from healthy controls were stimulated with IFNα or TLR7/8 or TLR9 agonists with or without HCQ.
Results: We found no differences in plasma IFNα levels of patients taking HCQ versus those not taking it, nor was there altered IFNα production following TLR stimulation. In SLE, persistent activation of T cell, TLR7/8, and TLR9 signaling leads to exhaustion of these pathways. Compared to controls, we confirmed reduced phosphorylation of multiple signaling proteins and reduced cytokines in patients on or off HCQ after stimulation by TLR agonists (Figure 1A and 1B). However, cytokine production following T cell or TLR stimulation was less impaired in patients on HCQ with an increased fold change in IL-10 (p=0.003), IFNg (p=0.011), IL-18 (p=0.016), CXCL13 (p=0.009), IL-6 (p=0.046), IL-1α (p=0.036) and other cytokines that approached healthy controls. The only cytokines that did not exhibit improved production in those on HCQ were IFNα and TNFα following TLR stimulation, where fold change was reduced in all SLE patients compared to healthy controls (p< 0.01). In control samples treated with HCQ in vitro, TLR9 induced signaling of p-p38 (p=0.046) and pIκBα (p=0.047) was reduced in plasmacytoid and myeloid dendritic cells. In SLE samples (where exhaustion of the TLR9 signaling pathway occurs) (Figure 1A and 1B), HCQ use was not associated with any further reduction or rescue of TLR9 signaling. However, IFNα signaling was diminished within the MAPK pathway (p=0.004) in SLE patients taking HCQ (Figure 1C), consistent with impeded Type I IFN signaling.
Conclusion: SLE is characterized by diminished cytokine production after prolonged T Cell and TLR stimulation. Once this occurs, HCQ has no observable impact on circulating or TLR-stimulated whole blood IFNα levels. However, rescue of some T Cell and TLR-driven cytokine production, and decreased signaling in the IFNα-induced MAPK pathway occurs in patients on HCQ. This suggests that TLR9 pathway exhaustion circumvents some, but not all, therapeutic activity of HCQ on Type I interferon-mediated pathology.
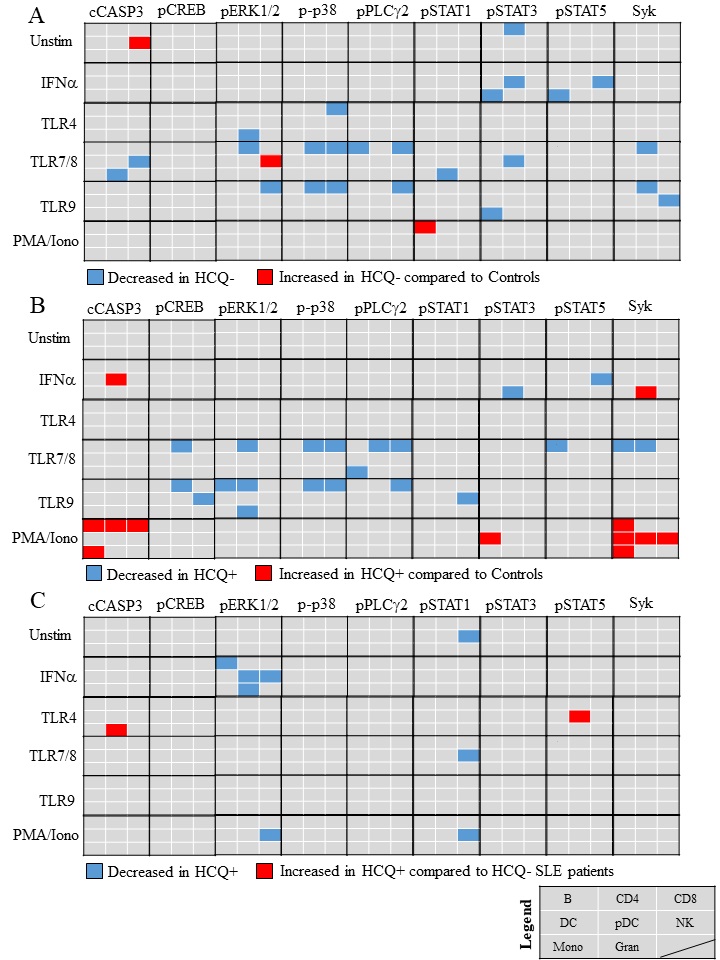 Figure 1. IFN-alpha signaling is diminished in SLE patients taking HCQ. Whole blood from either HCQ+ (SLE patients taking HCQ) or HCQ- SLE patients (SLE patients not taking HCQ) or healthy controls were stimulated for 15 minutes with either no stimuli, IFN-alpha, PMA and ionomycin, or TLR4, TLR7/8, or TLR9 agonists. The median 95th percentile was used to calculate the fold change of (A) HCQ- over controls (B) HCQ+ over controls or (C) HCQ+ over HCQ- in 8 cell populations (B cells, CD4+ T cells, CD8+ T cells, dendritic cells (DCs), plasmacytoid DCs (pDCs), natural killer (NK) cells, monocytes (mono) and granulocytes (gran). Significant increases or decreases in phophorylation following stimulation in a particular signaling molecule are noted by a blue box (decrease) or a red box (increase). The location of the box coincides with significant differences found in a specific cell population (refer to legend). p < 0.05
Figure 1. IFN-alpha signaling is diminished in SLE patients taking HCQ. Whole blood from either HCQ+ (SLE patients taking HCQ) or HCQ- SLE patients (SLE patients not taking HCQ) or healthy controls were stimulated for 15 minutes with either no stimuli, IFN-alpha, PMA and ionomycin, or TLR4, TLR7/8, or TLR9 agonists. The median 95th percentile was used to calculate the fold change of (A) HCQ- over controls (B) HCQ+ over controls or (C) HCQ+ over HCQ- in 8 cell populations (B cells, CD4+ T cells, CD8+ T cells, dendritic cells (DCs), plasmacytoid DCs (pDCs), natural killer (NK) cells, monocytes (mono) and granulocytes (gran). Significant increases or decreases in phophorylation following stimulation in a particular signaling molecule are noted by a blue box (decrease) or a red box (increase). The location of the box coincides with significant differences found in a specific cell population (refer to legend). p < 0.05
To cite this abstract in AMA style:
Slight-Webb S, Thomas K, Lu R, Macwana S, Merrill J, Arriens C, Chakravarty E, Aberle T, Maecker H, Utz P, Guthridge J, James J. Hydroxychloroquine Use Is Associated with Diminished Type I Interferon-related Pathways in Systemic Lupus Erythematosus Patients [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/hydroxychloroquine-use-is-associated-with-diminished-type-i-interferon-related-pathways-in-systemic-lupus-erythematosus-patients/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/hydroxychloroquine-use-is-associated-with-diminished-type-i-interferon-related-pathways-in-systemic-lupus-erythematosus-patients/
