Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Our current knowledge about how to treat lupus in pregnancy derives from small prospective or retrospective cohorts, and how best to manage lupus nephritis remains unknown. The goal of this individual participant meta-analysis was to pool data from multiple prospective cohorts to answer the clinical question of whether hydroxychloroquine (HCQ) treatment is beneficial from the decision point of the first trimester.
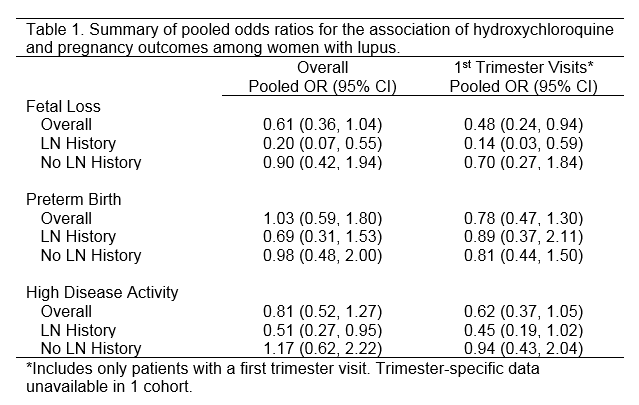
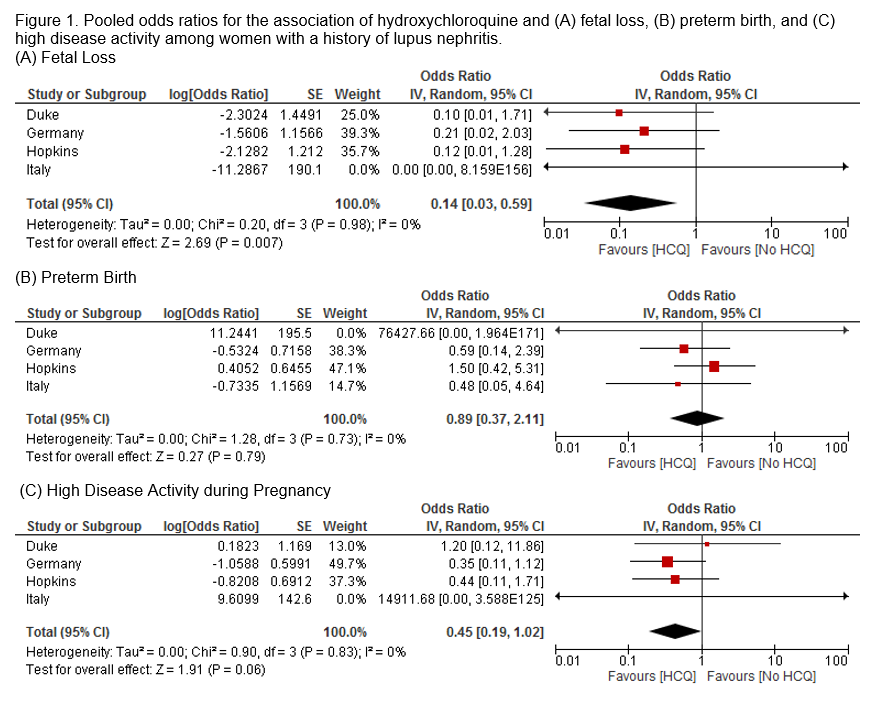
Methods: PubMed, Embase, and the Cochrane Database of Systematic Reviews were searched for prospective cohorts of pregnancies among women with lupus. Data from each cohort were collected and analyzed individually. HCQ use was defined as use any time during pregnancy. Outcomes of interest included fetal loss, preterm birth (<37 weeks gestation), and high disease activity (PGA ever >1, SLEDAI ever >4, or a report of a flare, depending on available data). Logistic regression models estimated log odds ratios (OR) and standard errors individually in all cohorts. Pooled ORs were calculated by random-effect models using the generic inverse variance method in Review Manager. Primary analysis included only women with first trimester visits (5 cohorts). Sensitivity analyses included all women (6 cohorts), and subgroup analyses included patients with a history of nephritis.
Results: 46 potential cohorts were identified from 2811 manuscripts. Seven cohorts met inclusion criteria and agreed to participate. The current analysis included 811 pregnancies from six cohorts, of which 70% were exposed to HCQ during pregnancy.
Fetal Loss: When limited to only patients with a 1st trimester visit, a 52% decrease in fetal loss was observed (OR: 0.48; 95% CI: 0.24, 0.94; Table 1). Among all patients there was a modest decrease in fetal loss among HCQ users, but the association was stronger among women with a history of nephritis (Figure 1).
Preterm Birth: No association with HCQ use during pregnancy and preterm birth was observed among women with a 1st trimester visit (OR: 0.78; 95% CI: 0.47, 1.30), among all women, and among women with nephritis.
Disease Activity: Among patients with a 1st trimester visit, there was a decrease in high disease activity among HCQ users (OR: 0.62; 95% CI: 0.37, 1.05), particularly among women with a history of nephritis. Among all patients, there was no association of HCQ use and high disease activity during pregnancy.
Conclusion: Our results suggest that HCQ may decrease the risk of fetal loss, and the benefits are seen most among women with nephritis. The heterogeneity of data collection suggests a unified approach to identify larger cohorts of lupus pregnancies is needed.
To cite this abstract in AMA style:
Eudy AM, Petri M, Fischer-Betz R, Mokbel A, Nalli C, Andreoli L, Tincani A, Molad Y, Balevic S, Clowse MEB. Hydroxychloroquine in Lupus Pregnancy: A Meta-Analysis of Individual Participant Data [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/hydroxychloroquine-in-lupus-pregnancy-a-meta-analysis-of-individual-participant-data/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/hydroxychloroquine-in-lupus-pregnancy-a-meta-analysis-of-individual-participant-data/