Session Information
Date: Friday, November 6, 2020
Title: Epidemiology & Public Health Poster I: COVID-19 & Rheumatic Disease
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Chloroquine (CQ) and hydroxychloroquine (HCQ) have been shown to have antiviral properties and were considered as potential therapeutic options amid the COVID-19 pandemic. The purpose of the current study is to evaluate the risk of hospitalization for viral infections among patients previously exposed (or not) to HCQ/CQ in the pre-COVID-19 era.
Methods: We studied adult rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE) individuals identified in the MarketScan database with an outpatient diagnosis (including emergency room, ER) of viral pneumonia or other viral acute respiratory infections. We required patients to be covered in the medical/pharmacy plan at least one year before time zero (date of outpatient infection). The main exposure was recent use of HCQ/CQ in the 90 days prior to time zero. We defined the outcome as hospitalization for viral infection within the 30 days after time zero. We used multivariate Poisson regression models with a robust error variance to estimate hospitalization in relationship to exposure to these drugs. Our models included demographic variables (age, sex), setting in which viral infection was initially identified (ER or other), underlying condition (RA or SLE), comorbidities, and use of other medications (modeled in the same way as the main exposure): methotrexate (MTX), mycophenolate (MMF), azathioprine, other DMARDs (cyclophosphamide, sulfasalazine, and leflunomide), corticosteroids, biologics, and NSAIDs. Analysis were combined for RA and SLE patients, but interaction terms were included to allow for the effect of HCQ to differ in the two conditions.
Results: We identified 63,971 episodes of outpatient infections among 54,561 RA/SLE patients. Baseline characteristics are presented in Table 1. Individuals were mostly women (80%), with average age of 57.4 years (standard deviation, SD 13.9). During the 30-day period following outpatient infection, we found 480 occurrences of hospitalization for viral respiratory infections. In adjusted multivariate analyses, we were unable to detect a clear difference in the risk of hospitalized viral infection when comparing recent versus non-recent use of HCQ/CQ in the past 90 days before the initial outpatient viral infection (adjusted RR: 0.89, 95% CI: 0.70–1.12; Table 2). In the same model, we found that comorbidity, ER presentation, older age, and MMF, azathioprine, and corticosteroids were all significantly associated with hospitalized viral infection.
Conclusion: While we saw no clear effect of HCQ/CQ, comorbidity, ER presentation, older age, and MMF, azathioprine, and corticosteroids were all significantly associated with hospitalized viral infection in RA and SLE.
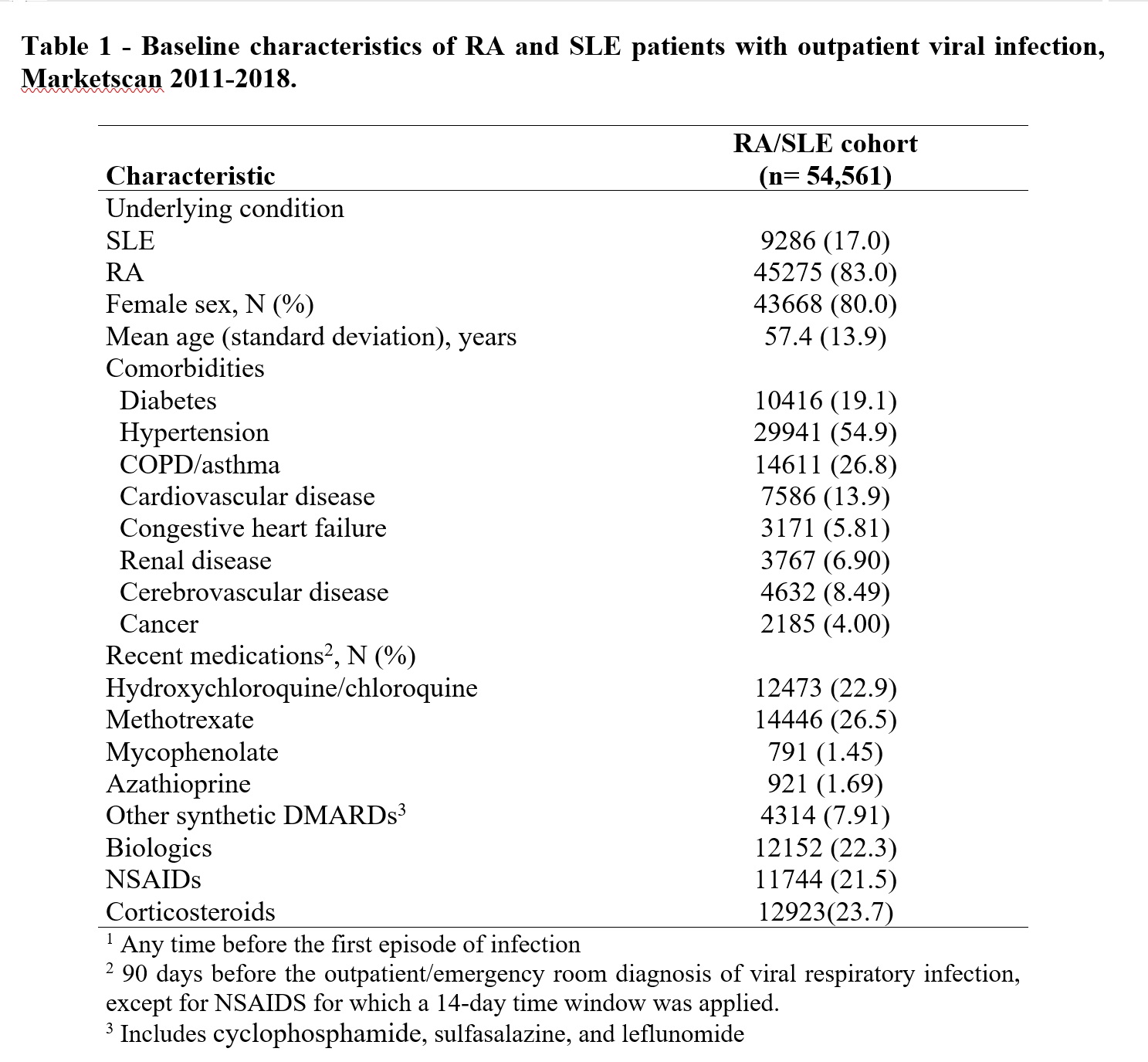 Baseline characteristics of RA and SLE patients with outpatient viral infection, Marketscan 2011-2018.
Baseline characteristics of RA and SLE patients with outpatient viral infection, Marketscan 2011-2018.
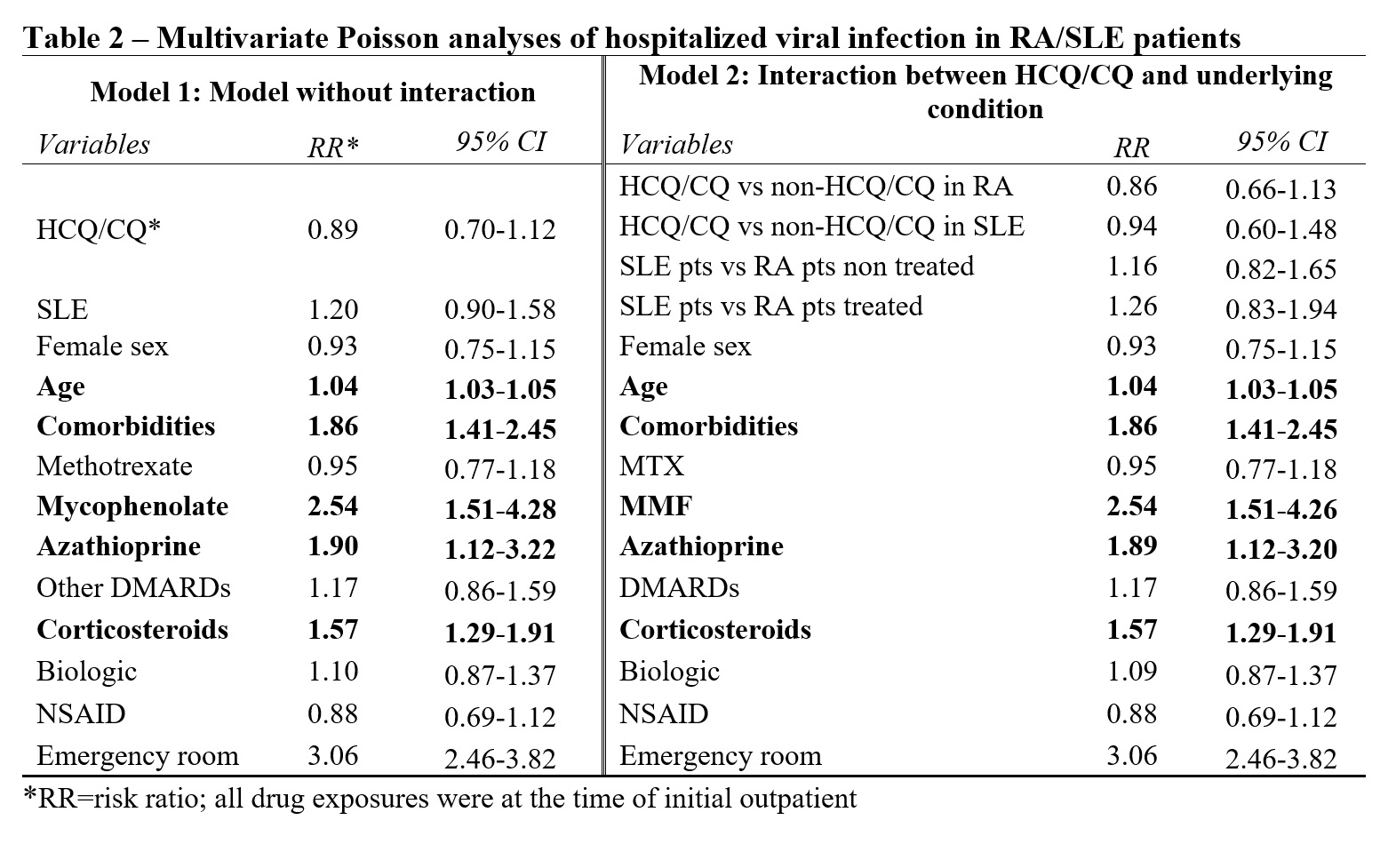 Multivariate Poisson analyses of hospitalized viral infection in RA/SLE patients
Multivariate Poisson analyses of hospitalized viral infection in RA/SLE patients
To cite this abstract in AMA style:
Moura C, Machado M, Almeida-Brasil C, Curtis J, Winthrop K, Abrahamowicz M, Bernatsky S. Hydroxychloroquine and Chloroquine and Hospitalizations for Viral Infection in the Pre-COVID-19 Era [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/hydroxychloroquine-and-chloroquine-and-hospitalizations-for-viral-infection-in-the-pre-covid-19-era/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/hydroxychloroquine-and-chloroquine-and-hospitalizations-for-viral-infection-in-the-pre-covid-19-era/
