Session Information
Session Type: ACR Plenary Session
Session Time: 11:00AM-12:30PM
Background/Purpose: Bone marrow lesions (BML) are well described in osteoarthritis (OA) and associate with pain, but little is known about histological and functional features of BMLs. We evaluated BMLs using novel tissue analysis tools to understand how they mediate pain.
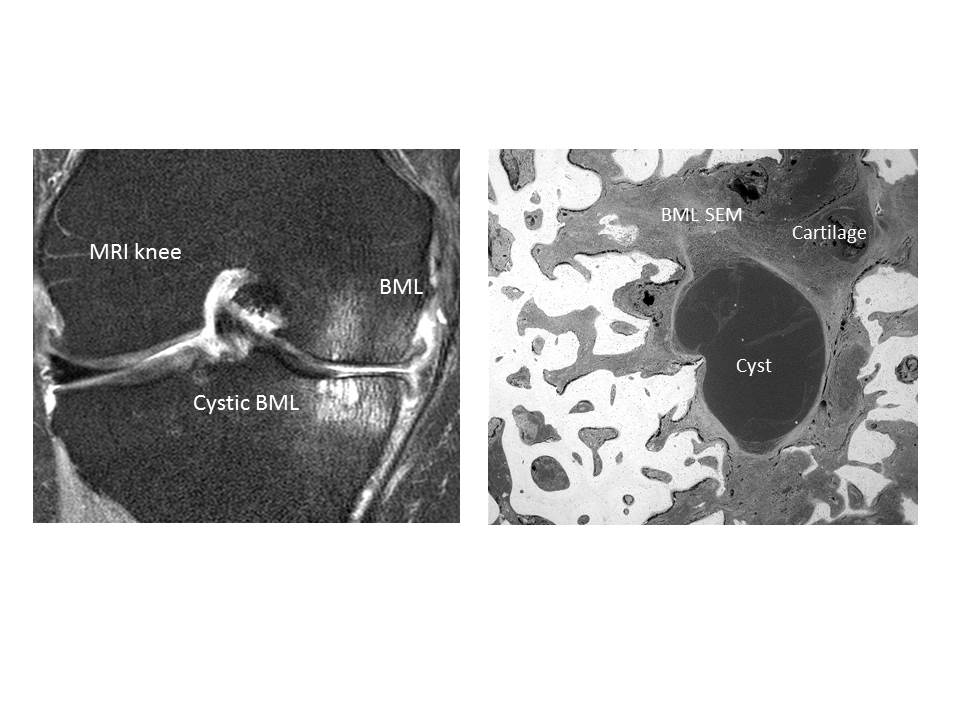
Methods: Subjects fulfilling ACR criteria for knee OA were recruited with early and advanced OA with matched controls (n=96). Advanced OA subjects had a total knee replacement (TKR)(n=72). Early knee OA subjects had pain but did not require surgery (n=12). Controls (n=12) were recruited for pain measures and tissue comparisons from non-OA knee surgery. All subjects were assessed by Western Ontario and MacMaster Universities Osteoarthritis Index (WOMAC). Participants had knee MRI to define BML characteristics and tissue damage. Tissue was harvested at TKR for BML analysis using scanning electron microscopy (SEM) and tissue microarray using Illumina. For SEM, tissue blocks were embedded in poly (methylmethacrylate) to give intact tissue and analysed to obtain 3 Dimensional SEM. For microarray, RNA was isolated and reverse transcribed using the Qiagen system and subjected to microarray.
Results: The mean (SD) total WOMAC scores in the groups were: advanced OA 1436.2 (471.6), early OA 797.4 (549.6) and controls 10.5 (12.6), demonstrating that the advanced OA group had severe pain (p<0.0001). MRI scoring in the advanced OA group showed all had tibial and femoral BMLs. SEM found most normal bone marrow was adipocytic with adipocytes the major bone lining cells, making and moulding trabecular excrescences. Bone volume fraction was starkly reduced in BMLs, with marrow replaced by dense fibrous connective tissue, hyaline cartilage and fibrocartilage. Aggressive resorption was found at the periphery of BML patches and areas of calcified cartilage deep in the bone, arising by mineralisation of cartilage formed within the bone organ (Figure 1). Microarray of 24 samples from the knee OA BMLs and controls showed 218 genes were differentially regulated compared with control samples (p<0.05). Gene groups demonstrating highest levels of regulation included extracellular matrix proteins, thrombospondin 4, chondrocyte-expressed matrix metalloproteinases (MMP-13), neuro-epithelial and axonal development proteins, pro-inflammatory cytokines and catenin signalling.
Conclusion: Our work is the first to employ SEM and microarray in one study to interrogate OA BMLs. We have found that BMLs demonstrate areas of high metabolic activity, expressing cartilage proteins and enzymes in addition to neuronal differentiation proteins which could explain why they are strongly associated with pain.
To cite this abstract in AMA style:
Sofat N, Assi L, Kuttapitiya A, Boyde A, Ejindu V, Heron C. How Do Bone Marrow Lesions Cause Osteoarthritis Pain? a Structural and Functional Tissue-Based Study [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/how-do-bone-marrow-lesions-cause-osteoarthritis-pain-a-structural-and-functional-tissue-based-study/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/how-do-bone-marrow-lesions-cause-osteoarthritis-pain-a-structural-and-functional-tissue-based-study/