Session Information
Date: Tuesday, November 12, 2019
Title: Systemic Sclerosis & Related Disorders – Clinical Poster III
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Systemic sclerosis (SSc) is an autoimmune disorder associated with multi-organ dysfunction, requiring long-term and multi-disciplinary care. Few studies have estimated the healthcare resource usage of patients with SSc. The purpose of this study was to compare hospitalization among incident cases of SSc vs age- and sex-matched comparators.
Methods: A retrospective, population-based cohort of physician-diagnosed patients with SSc in a geographically well-defined area from Jan 1, 1980 to Dec 31, 2016 was identified and utilized for this study. A 2:1 cohort of age- and sex-matched non-SSc subjects from the same population was randomly selected for comparison. Patients who died or emigrated from the area prior to 1987 were excluded. Patients were followed until death, migration from the geographic area or Sep 30, 2018. All hospitalizations in the geographic area from Jan 1, 1987 to Sep 30, 2018 were obtained. Primary discharge diagnosis information was available for hospitalizations in 1995 to present. Readmission was defined as occurring within 30 days of a discharge. Rates of hospitalization of cases and comparators were analyzed using person-year methods and rate ratios. Length of stay was analyzed using generalized linear models adjusted for age, sex and calendar year, with random intercepts to account for multiple hospitalizations per patient.
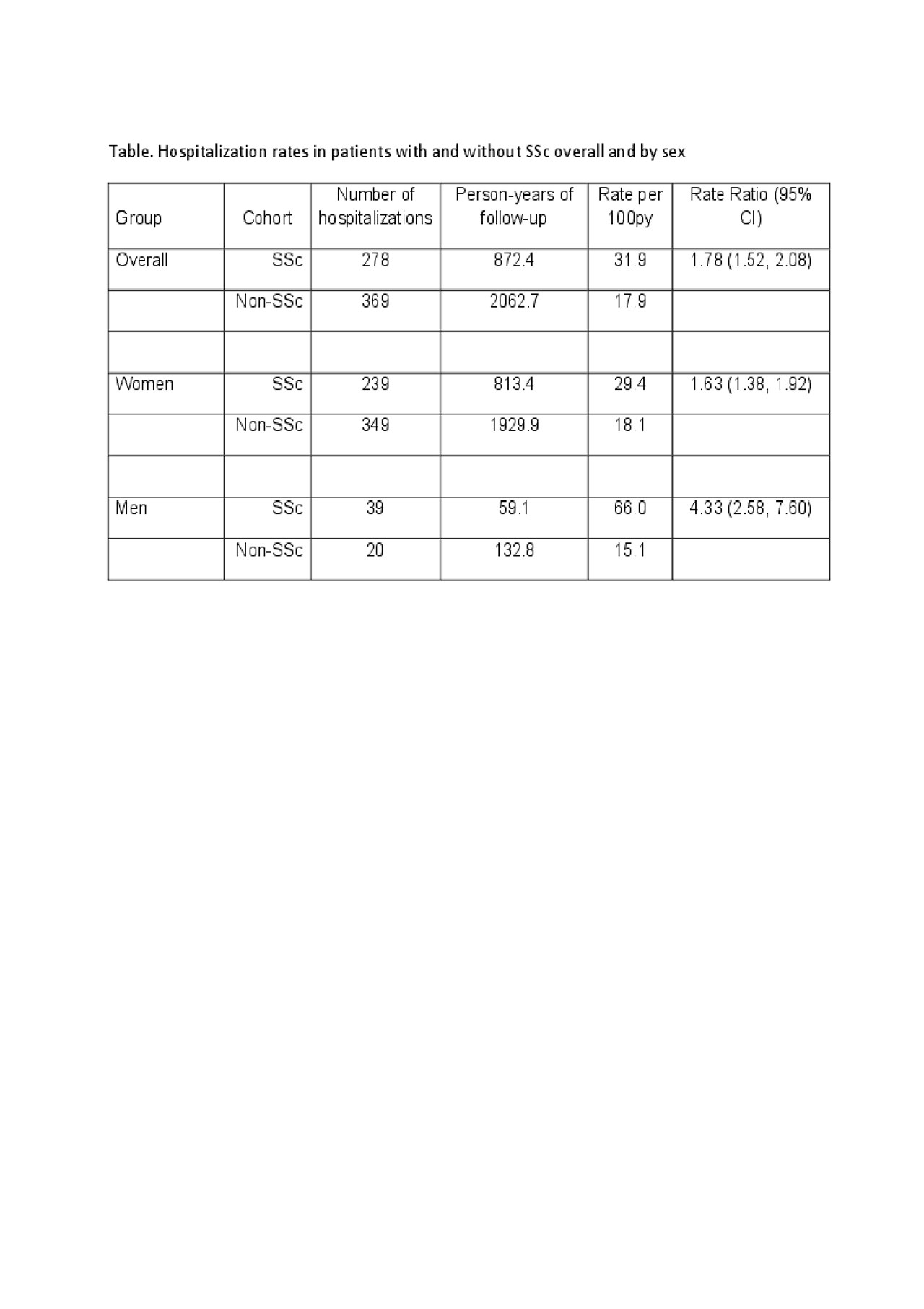
Results: The cohort included 76 incident SSc cases and 155 non-SSc comparators (mean age of 56 ± 16 years at diagnosis/index, both 91% female). Mean length of follow-up was 11.5 (SD 8.5) years for SSc subjects and 13.3 (SD 8.6) years for comparators. Rates of hospitalization among cases and comparators were 31.9 and 17.9 per 100 person-years, respectively (rate ratio [RR]:1.78; 95% confidence interval (CI):1.52-2.08)(Table). By sex, men (RR:4.33; 95%CI:2.58-7.60) and women (RR:1.63; 95%CI:1.38-1.92) with SSc had substantially higher hospitalization rates than comparators.
Hospitalization rates were higher in SSc compared with non-SSc subjects during the first 5 years after SSc diagnosis (RR: 2.16; 95%CI:1.70-2.74). This difference decreased over time and was no longer significant for ≥15 years after SSc incidence/index (Figure). Patients age 65+ were more frequently hospitalized than younger subjects in both SSc and comparator groups, and the difference in hospitalization rates between groups was largest in those age < 50 years (RR: 2.54: 95% CI: 1.73-3.75).
SSc subjects were more frequently hospitalized for infections and diseases involving circulatory, digestive, and respiratory systems than comparators, with ratios ranging from 1.96 to 3.90. Lengths of stay (median (IQR) 4 (2-6) vs 3(2-6); p=0.52) and readmission rates (25% vs 23%; p=0.51) were similar among cases and comparators.
Conclusion: A higher frequency of hospitalization occurred among patients with SSc compared to non-SSc subjects, indicating high inpatient care needs in this population. Hospitalization rates were highest among SSc subjects during the first 5 years of SSc diagnosis. Hospitalization rates approached those of non-SSc comparators over time after diagnosis, possibly due to confounding by age and other comorbidities.

HospitalizationFigure5.31.2019
To cite this abstract in AMA style:
Coffey C, Sandhu A, Crowson C, Achenbach S, Matteson E, Osborn T, Warrington K, Makol A. Hospitalization Among Incident Cases of Systemic Sclerosis: Results from a Population-based Cohort (1980-2016) [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/hospitalization-among-incident-cases-of-systemic-sclerosis-results-from-a-population-based-cohort-1980-2016/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/hospitalization-among-incident-cases-of-systemic-sclerosis-results-from-a-population-based-cohort-1980-2016/