Session Information
Date: Tuesday, November 19, 2024
Title: Abstracts: SLE – Diagnosis, Manifestations, & Outcomes III: Targets, Outcomes & Comorbidity
Session Type: Abstract Session
Session Time: 11:00AM-12:30PM
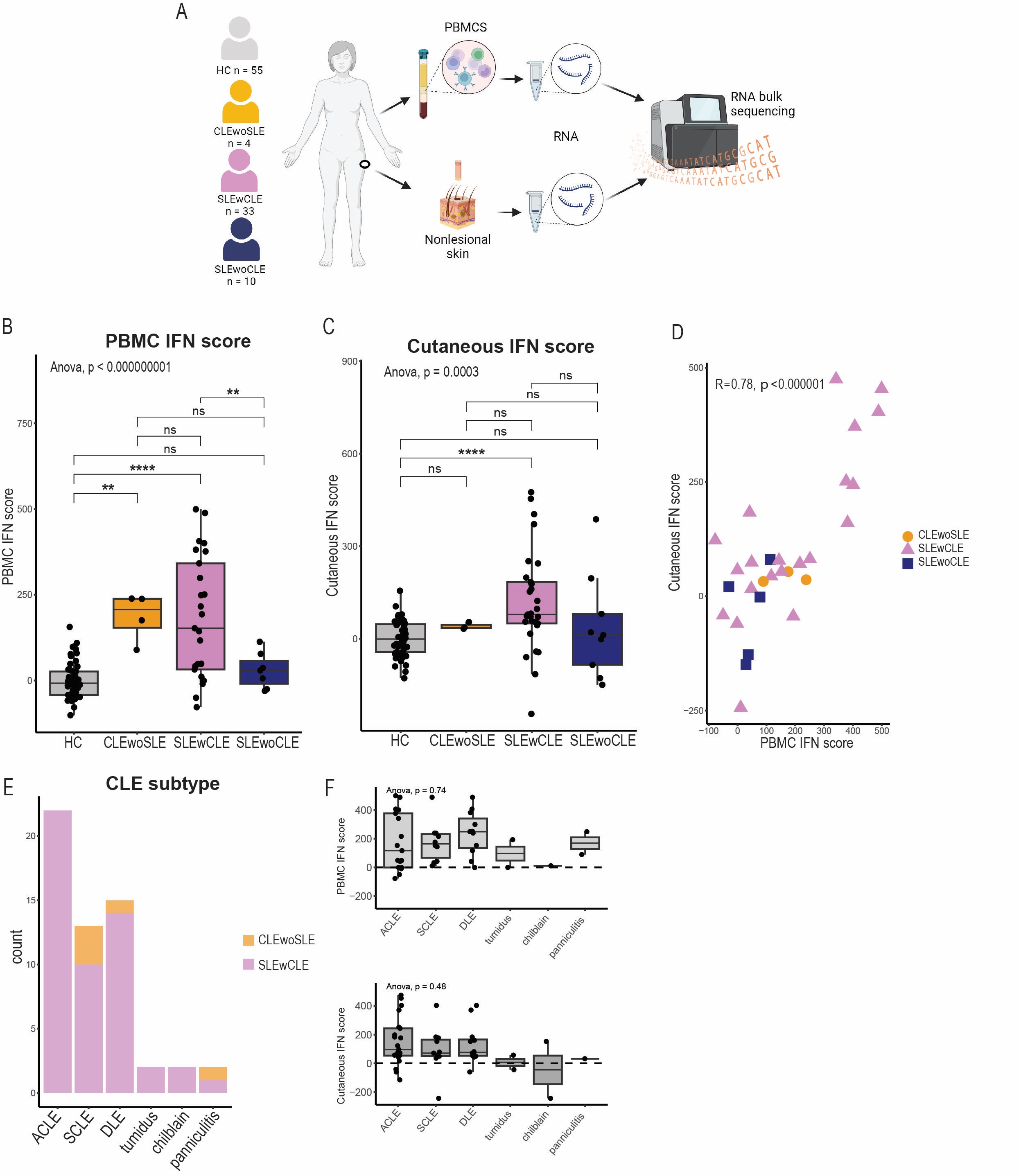
Background/Purpose: Cutaneous lupus (CLE) can present in isolation or as one of the most common manifestations of systemic lupus erythematosus (SLE). Interferon (IFN) stimulated genes (ISGs) are highly expressed in CLE lesions and in circulating blood cells from SLE patients. Importantly, ISGs are also increased in non-lesional, healthy appearing skin of SLE patients. However, it is unknown whether this is different in SLE patients with and without cutaneous involvement and how ISG expression in non-lesional skin relates to ISGs in blood. Here, we compared ISGs in non-lesional skin and PBMCs between patients with or without a history of CLE.
Methods: For this cross-sectional study, we performed bulk RNA sequencing of non-lesional, not sun-exposed skin and PBMCs of in total 33 SLE patients with a history of cutaneous lupus (SLEwCLE), 10 SLE patients without a history of cutaneous involvement (SLEwoCLE), 4 patients with a history of cutaneous lupus without SLE (CLEwoSLE) and 55 healthy controls (HC). All SLE patients met the EULAR-ACR criteria. The expression of selected ISGs was summarized as IFN-scores (Z-scores), consisting of 138 genes that were upregulated after stimulating keratinocytes with IFNα. For paired skin and PBMC samples, we tested for correlation between PBMC and non-lesional, cutaneous IFN scores. In addition, differential gene expression and gene set enrichment analysis (GSEA) was performed.
Results: PBMCs from CLEwoSLE and SLEwCLE had higher IFN scores compared to HC, while PBMCs from SLEwoCLE did not exhibit increased IFN scores. Similarly, SLEwCLE showed the highest IFN scores in non-lesional skin among all groups. This effect seemed to be independent of CLE subtype. GSEA showed ISGs to be the most significantly upregulated genes when comparing SLEwCLE to HC and SLEwoCLE patients. Furthermore, IFN scores from PBMCs and non-lesional skin were strongly correlated (r = 0.78). Cutaneous and PBMC interferon scores were neither associated with disease activity (SLEDAI) nor with cutaneous lupus disease activity (CLASI).
Conclusion: ISGs in non-lesional skin and PBMCs were elevated in lupus patients with a history of CLE compared to patients without skin involvement, suggesting different pathophysiological mechanisms between patients with and without CLE. Non-lesional skin and PBMC interferon signatures were strongly correlated, supporting that the non-lesional skin is an immune activated site that has strong interplay with the systemic immune system.
Abbreviations: HC: healthy controls; CLEwoSLE: cutaneous lupus patients without systemic lupus erythematosus; SLEwCLE: systemic lupus erythematosus patients with a history of cutaneous lupus; SLEwoCLE: systemic lupus erythematosus patients without a history of cutaneous lupus; IFN: interferon; PBMC: peripheral blood mononuclear cells; CLE: cutaneous lupus; ACLE: acute cutaneous lupus erythematosus; SCLE: subacute cutaneous lupus erythematosus; DLE: discoid lupus erythematosus; ns: not significant; * : p < 0.05; **: p < 0.01; *** p < 0.001, **** p < 0.0001.
Image A was created with BioRender.com
To cite this abstract in AMA style:
Henning S, Tsoi L, Dobry C, Berthier C, Klein B, Hurst A, Wasikowski R, Gudjonsson J, Kahlenberg J. History of Cutaneous Lupus Promotes Blood and Skin Interferon Signatures in SLE Patients [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/history-of-cutaneous-lupus-promotes-blood-and-skin-interferon-signatures-in-sle-patients/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/history-of-cutaneous-lupus-promotes-blood-and-skin-interferon-signatures-in-sle-patients/