Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE) are complex autoimmune diseases associated with pain and decreased quality of life. Mental health conditions related to stress and emotional distress, in particular depression, anxiety, and post-traumatic stress disorder (PTSD), appear to be common among those with these rheumatic diseases, but estimates in large diverse populations are not yet available. We assessed the prevalence of these three mental health conditions among patients with RA and SLE, comparing them to those without in a large and diverse healthcare center-based nationwide cohort.
Methods: We conducted a cross-sectional study within the All of Us Research Program, an ongoing NIH-funded cohort that enrolled US adults age ≥18 from May 6, 2018 – July 1, 2022 (release v7). It includes consented electronic health record (EHR) data for >287,000 people. RA and SLE patients were identified by ≥ 2 International Classification of Diseases (ICD)-9, ICD-10, and Systematized Nomenclature of Medicine (SNOMED) codes >2 months apart but within ≤2 years prior to enrollment. Depression, anxiety, and PTSD were also identified by ICD-9 or-10, and SNOMED codes within 1 year prior to enrollment. Prevalence of each mental health disorder among patients with RA and SLE was compared to age-, sex-, and race/ethnicity-matched patients (1:4 matched). Conditional logistic regression models estimated odds ratios (ORs) for these mental health conditions, adjusting sequentially for socioeconomic factors (Model 1), + smoking, obesity, and other comorbidities (Model 2). Age-stratified analysis was performed for groups aged 18-44, 45-64, and ≥65 years.
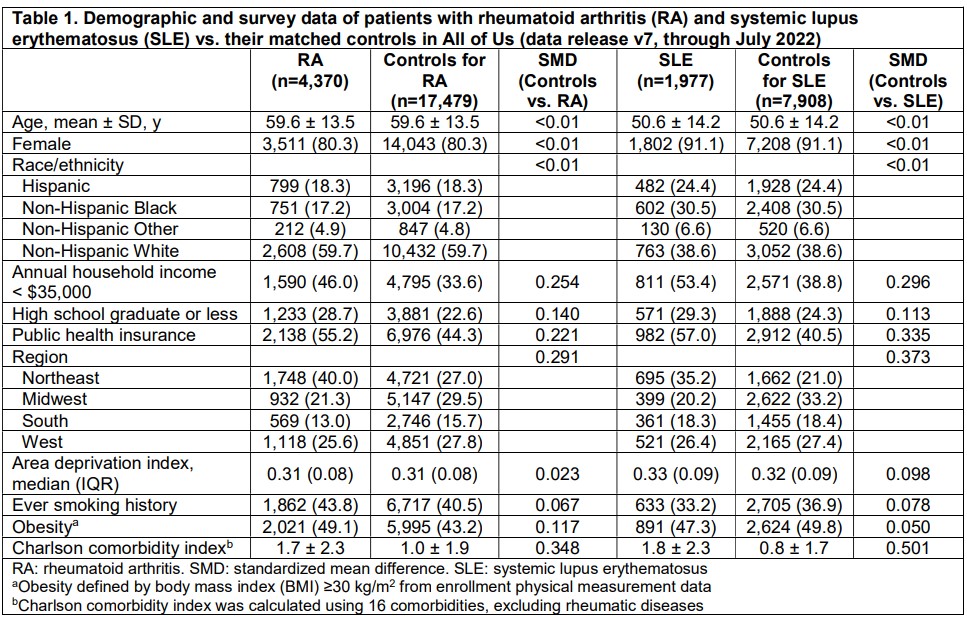
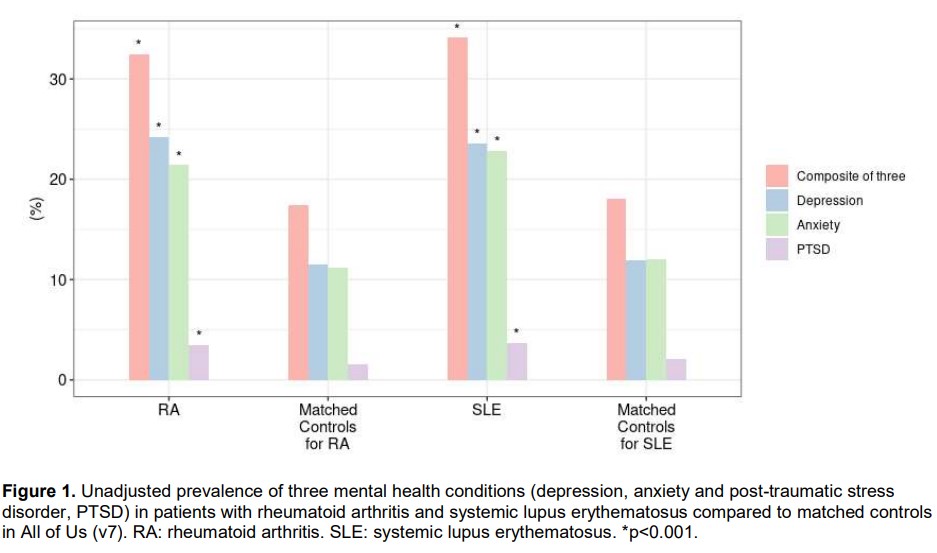
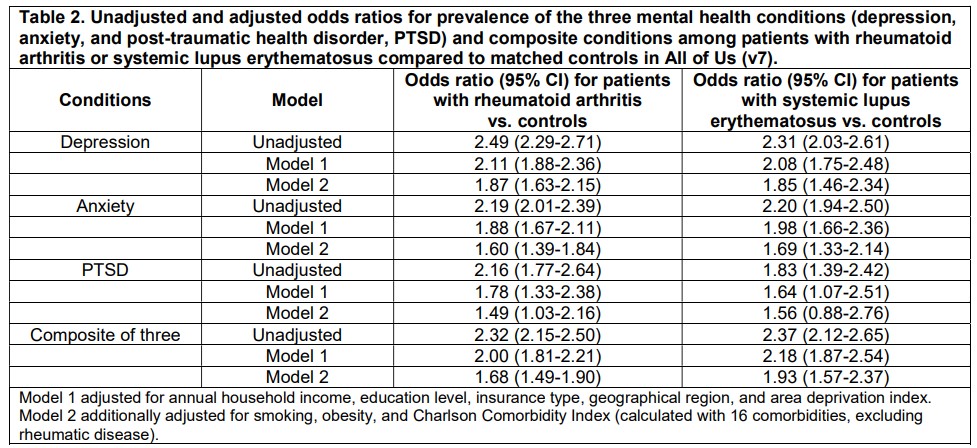
Results: After matching for age, sex, and race/ethnicity, we studied 4,370 RA patients, 1,977 SLE patients, and their matched controls (17,479 for RA; 7,908 for SLE) (Table 1). Both RA and SLE patients had lower educational attainment, and were less frequently privately insured, and more comorbidities than their matched controls. Compared to controls, RA patients had higher prevalence of depression (24.2 % vs. 11.5%), anxiety (21.4% vs. 11.2%), and PTSD (3.5% vs. 1.6%) (Figure 1). Similarly, compared to controls, SLE patients had higher prevalence of depression (23.6% vs. 11.9%), anxiety (22.8% vs. 12.0%), and PTSD (3.7% vs. 2.1%). Table 2 shows sequential modeling results. While adjusting for potential confounders, which attenuated the ORs, RA patients vs controls had 1.7-fold (95% CI 1.5-1.9) higher odds of these mental health conditions in fully-adjusted models. For SLE patients, the adjusted OR was 1.9 (95% CI: 1.6-2.4). In the age-stratified analysis, the adjusted ORs were similar in each group, ranging from 1.5 to 1.8 in RA patients and from 1.8 to 2.3 in SLE patients.
Conclusion: Patients with RA and those with SLE had elevated prevalence of mental health conditions related to stress, trauma, and emotional distress than controls in the year prior to their cohort enrollment. These highly prevalent stress-related mental health conditions may complicate the care and treatment of rheumatic diseases. Research is ongoing to understand how mental health treatments affect rheumatic disease outcomes.
To cite this abstract in AMA style:
Yee J, Feldman C, Oakes E, Karlson E, Ellrodt J, Kubzansky L, Koenen K, Costenbader K. High Prevalence of Mental Health Disorders Among Patients with Rheumatoid Arthritis and Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/high-prevalence-of-mental-health-disorders-among-patients-with-rheumatoid-arthritis-and-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/high-prevalence-of-mental-health-disorders-among-patients-with-rheumatoid-arthritis-and-systemic-lupus-erythematosus/