Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Over 100 million adults have chronic pain, largely affecting older adults who often have >1 chronic pain condition. Traditionally, chronic overlapping pain conditions (COPC) are defined based on “functional” disorders such as fibromyalgia, irritable bowel syndrome, temporomandibular joint dysfunction, but such a characterization fails to incorporate musculoskeletal (MSK)-related pain. Further, the definition of widespread pain misses chronic MSK pain among those without axial pain. We sought to evaluate the prevalence of chronic multisite pain in older adults regardless of underlying diagnosis.
Methods: We included participants from a NIH-funded ancillary study to the Framingham Heart Study (FHS)’s 2nd generation 11th Exam (2019-2021), a community-based cohort of older adults unselected for pain or medical conditions, and oldest cohort in the world to have pain data. We obtained information about locations of pain using a body homunculus to catalogue MSK (joint and axial) pain, the Widespread Pain Index to identify non-articular pain locations, pain severity and duration, comorbidities, and pain medication use. We defined chronic pain as pain present >3months per the International Association for the Study of Pain definition. Chronic multisite pain was defined as ≥3 distinct body sites with chronic pain as per the traditional definition of COPC. Widespread pain was defined as pain above and below the waist, on the right and left sides of the body, and axial pain. We assessed prevalence of different aspects of pain, and NSAID use by presence of contraindicated or precautionary comorbidities.
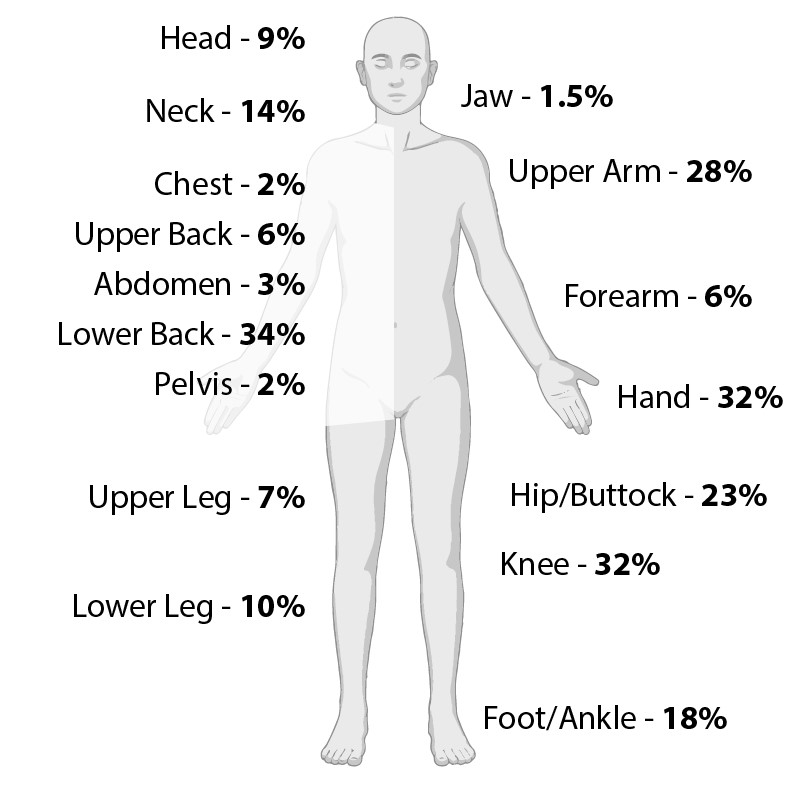
Results: We evaluated 1613 participants (mean (±SD) age 76±7.5, 56% females, mean (±SD) BMI 28.0±5.2). In the whole cohort, 33% reported pain severity ≥4/10 (threshold typically used for enrolment into pain randomized trials), 78% reported ≥1 site of pain, 52% had chronic pain, 34% had chronic multisite pain, 19% met the definition of widespread pain, and 43% reported using NSAIDs (only 1% was topical) and 3% opioids. Of those who reported ≥1 site of pain, 93% reported pain in MSK locations; the most common were knee, hand, and low back (each >30%) (Figure 1). Notably, ~75% who reported chronic multisite pain had cardiovascular disease, renal disease, or gastroesophageal conditions, and >50% of them reported using oral NSAIDs despite having these comorbidities; these proportions of NSAID use were higher among those with chronic multisite pain than those without.
Conclusion: This study provides the first comprehensive pain data among much older adults than typically studied. Among these older adults living in the community, the prevalence of chronic multisite pain was high, and virtually all of the reported pain was in MSK locations. Of concern, over 50% with chronic multisite pain used NSAIDs despite having contraindications or comorbidities that warrant precautions with this class of agent, underscoring the challenge of pain management in the setting of a paucity of safe and effective management options. These data highlight the underrecognized and understudied substantial burden of MSK pain among older adults.
To cite this abstract in AMA style:
Dhamne S, Edwards R, Benjamin E, Tilley S, Demalia A, Clancy M, Gheller M, Neogi T. High Prevalence of and Medication Use in Musculoskeletal and Chronic Multisite Pain in Community-Dwelling Older Adults: The Framingham Heart Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/high-prevalence-of-and-medication-use-in-musculoskeletal-and-chronic-multisite-pain-in-community-dwelling-older-adults-the-framingham-heart-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/high-prevalence-of-and-medication-use-in-musculoskeletal-and-chronic-multisite-pain-in-community-dwelling-older-adults-the-framingham-heart-study/