Session Information
Date: Friday, November 6, 2020
Title: RA – Diagnosis, Manifestations, & Outcomes Poster I: Multimorbidity
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Nonalcoholic fatty liver disease (NAFLD), a spectrum of disorders characterized by the presence of hepatic steatosis, is the most common liver disorder in western countries. Risk factors, such as obesity, hypertension, dyslipidemia, insulin resistance, and elevated inflammatory cytokines, are frequent in RA. However, few prior studies have explored the prevalence and contributors to hepatic steatosis in RA.
Methods: A total of 235 RA patients underwent abdominal computed tomography (CT), with attenuation of hepatic parenchyma (away from hepatic vasculature) measured in Hounsfield units (HU). A cohort of 6615 non-RA controls underwent similar scanning and liver HU assessment. Any steatosis was defined as HU< 48. Moderate/severe hepatic steatosis was defined as HU< 40, a standard that correlates histologically with ≥30% fatty deposition. Generalized linear models were used to compare the prevalence of steatosis between the RA and control groups, adjusted for pertinent confounders, and to assess the associations of RA characteristics and other risk factors with steatosis within the RA group.
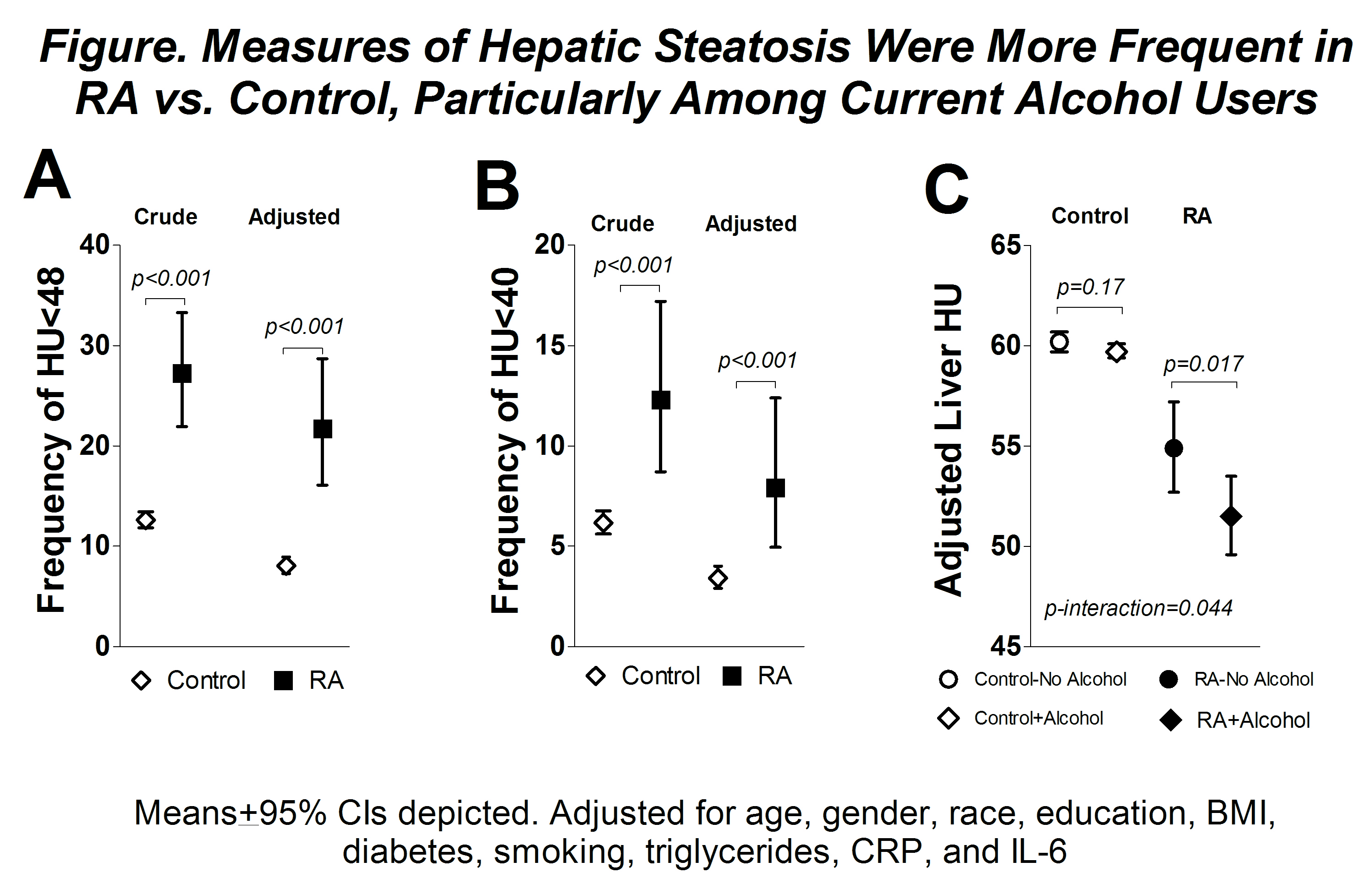
Results: Mean hepatic attenuation was 15% lower in the RA group compared with controls (51 vs. 60 HU, respectively; p< 0.001). The prevalence of any steatosis in RA was more than double that of controls (27 vs. 13%, respectively; p< 0.001) and remained significantly higher after adjusting for relevant confounders (adjOR=3.2; p< 0.001) (Fig 1A). The prevalence of moderate/severe steatosis was double that of the controls (12 vs. 6%, respectively; p< 0.001) and also remained significantly higher after adjustment (adjOR=2.5; p< 0.01) (Fig 1B). Alcohol consumption was more strongly linked to steatosis in the RA group compared with the control group (Fig 1C). RA patients with any steatosis had significantly higher CRP levels, on average, compared with RA patients without steatosis (9.3 vs. 4.4 mg/L, respectively; p< 0.001). Rheumatoid factor was more frequent among RA patients with any steatosis (84 vs. 66%, respectively; p=0.01). However, steatosis was not associated with articular disease activity nor current use of corticosteroids, or biologic and non-biologic DMARDs, including methotrexate and leflunomide.
Conclusion: Hepatic steatosis was more frequent in RA compared with controls, even after adjusting for relevant confounders, and was linked with autoimmunity and systemic inflammation. Current use of DMARDs was not associated with hepatic steatosis. Prospective studies will help elucidate the consequences of increased hepatic steatosis in RA patients and define whether intervention is warranted.
To cite this abstract in AMA style:
Lee J, Lagos G, Bathon J, Giles J. Hepatic Steatosis in Rheumatoid Arthritis: Frequency and Disease-Related Contributors [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/hepatic-steatosis-in-rheumatoid-arthritis-frequency-and-disease-related-contributors/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/hepatic-steatosis-in-rheumatoid-arthritis-frequency-and-disease-related-contributors/