Session Information
Date: Friday, November 6, 2020
Title: Miscellaneous Rheumatic & Inflammatory Diseases Poster I: Diagnosis and Testing
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Hemophagocytic syndrome (HPS) is classified into primary and secondary. The secondary form is mainly associated with hematological malignancies (HN) such as lymphomas, and autoimmune diseases (AI) such as Systemic Lupus Erythematosus. The mortality rate varies between 20% and 90%. Underlying malignancies, thrombocytopenia, age, hyperferrhythmia and prolonged prothrombin time are considered an adverse prognostic factor. The present work aims to obtain clinical and laboratory findings that can guide us to an early etiological diagnosis and treatment.
Methods: This is a retrospective observational study, which was approved by the hospital’s ethics committee. Any patient who met the diagnostic criteria for LHH proposed by Henter JI. or who presented hemophagocytic cells (HC) in bone marrow (BM) biopsy were included. We describe and identify clinical, laboratory findings and underlying disorder differences between HPS subgroups; and between patients who survived and did not survive to HPS at a tertiary hospital between 2005 and 2019. Continuous variables are described with the mean or median according to the degree of normality, and qualitative variables are shown with the absolute value and percentage. Kruskal Wallis, Fisher test and Mann-Whitney U test were used for the bivariate analysis.
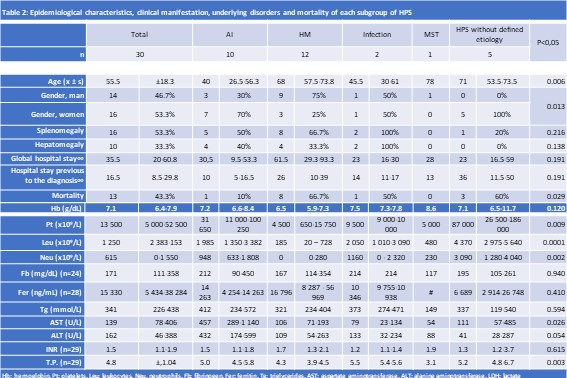
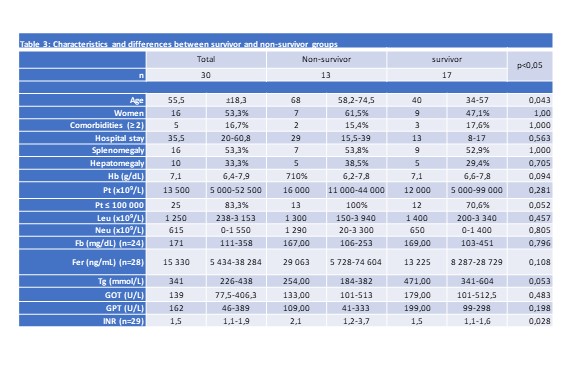
Results: Thirty patients were found (Table 1). The coincidence of an infectious disease with HPS was observed in 8 [AI: 5 cases (2 cytomegalovirus, 2 probably viral respiratory infections and 1 bacterial infection) and HM: 3 cases (2 Epstein Barr virus and 1 bacterial infection)]. In 2 patients with acute leukemia, allogeneic transplantation was related as a possible trigger of HPS; and in one patient with myelodysplastic syndrome it was related to the appearance of graft-versus-host disease. Age at diagnosis of HPS was lower in the AI subgroup [40 (26.5 – 56.3); p 0.001]. The HM subgroup presented more severe cytopenias [platelets 4500 (650 – 15 750; p 0.009), leukocytes 2050 (20 – 728; p 0.0001) and neutrophils 0 (0 – 280; p 0.002)] (table 2). Overall intra-hospital mortality was 43.3%, being higher in the HM subgroup [8 patients (66.7%); p 0.029]. The group of patients who did not survive had a longer time of prolongation of the INR compared to those who survived [2.1 (1.2 – 3.7) versus 1.5 (1.1 – 1.6); p 0.028] and an older age at diagnosis of HPS compared to the group who survived [68 years (58.2 – 74.5) versus 40 years (34 – 57); p 0.043] (Table 3).
Conclusion: The HM subgroup had higher mortality, and more and more severe cytopenias. The AI subgroup showed higher transaminase elevation and better prognosis. The non-survivor group had a longer time of prolongation of the INR and an older age at the time of the diagnosis of HPS compared to the survivor group.
To cite this abstract in AMA style:
Egües Dubuc C, Calvo-Alén J, de Diego Sola A, Cabrera-Miranda E, Alcorta N, Lopez Dominguez L, Maiz O, Uriarte Isacelaya E, Cancio Fanlo J, Valero Jaimes J, Belzunegui J. Hemophagocytic Syndrome. Clinical Characteristics and Prognostic Factors of a Series of 30 Clinical Cases [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/hemophagocytic-syndrome-clinical-characteristics-and-prognostic-factors-of-a-series-of-30-clinical-cases/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/hemophagocytic-syndrome-clinical-characteristics-and-prognostic-factors-of-a-series-of-30-clinical-cases/