Session Information
Date: Friday, November 6, 2020
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: The Health Assessment Questionnaire Disability Index (HAQ-DI) has been validated and widely used in psoriatic arthritis (PsA) clinical trials for the assessment of patient functional status. Few US studies have evaluated the economic impact of functional disability in patients with PsA. The purpose of this study was to evaluate the association of functional status with healthcare resource utilization (HCRU) and medical costs in US patients with PsA in a national data registry.
Methods: FORWARD is a longitudinal observational databank for rheumatic diseases that collects patient-reported data through questionnaires administered every 6 months. Data collected include demographics, clinical characteristics, symptoms, health and functional status, health-related quality of life, and HCRU. This cohort study included adult patients with PsA enrolled in FORWARD between July 2009 and June 2019 who completed ≥ 1 questionnaire, including the HAQ-DI, between January 2010 and December 2019. Patient demographics, clinical characteristics, and patient-reported outcomes were collected from the most recent questionnaire. HCRU and medical costs (USD 2019) for all hospitalizations, emergency department (ED) visits, outpatient visits, diagnostic tests, and procedures were assessed for the 6 months prior to survey completion. Negative binomial regression models (HCRU outcomes) and generalized linear models with gamma distribution and log-link function (cost outcomes) were used to assess the relationship between HAQ-DI and HCRU and cost outcomes adjusted for confounders.
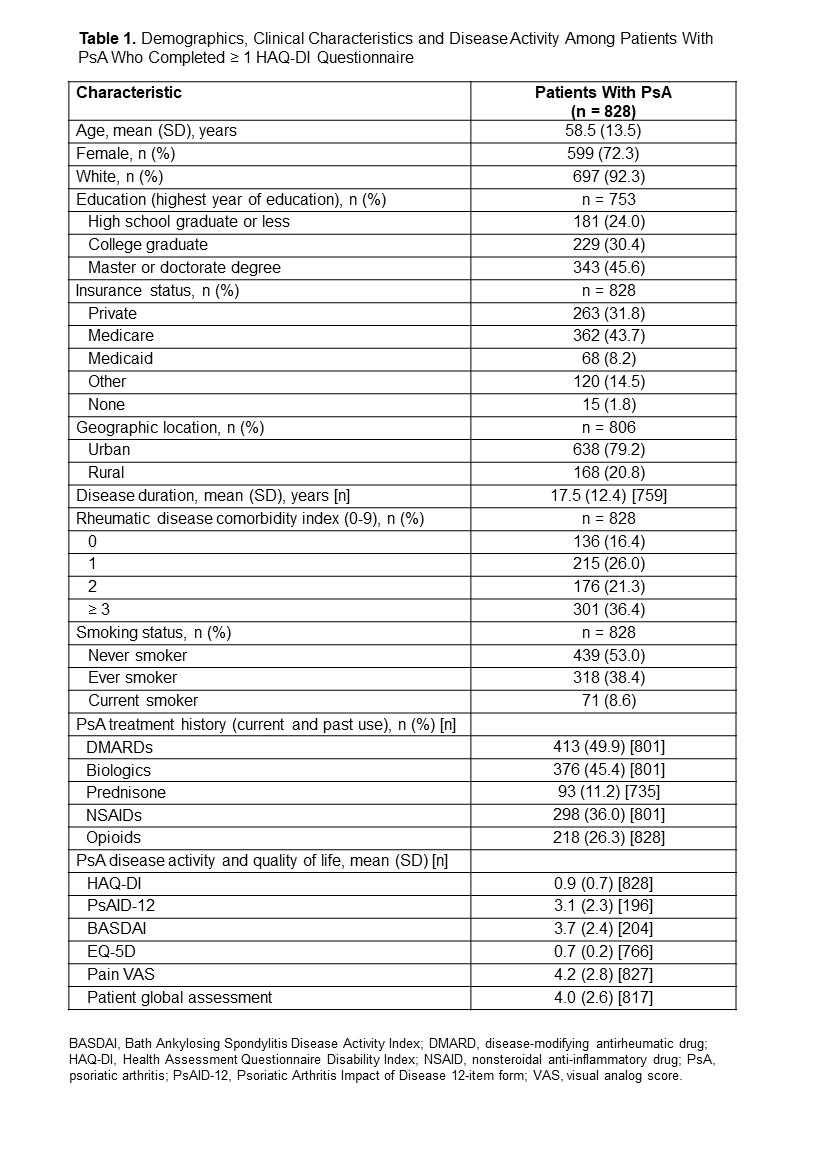
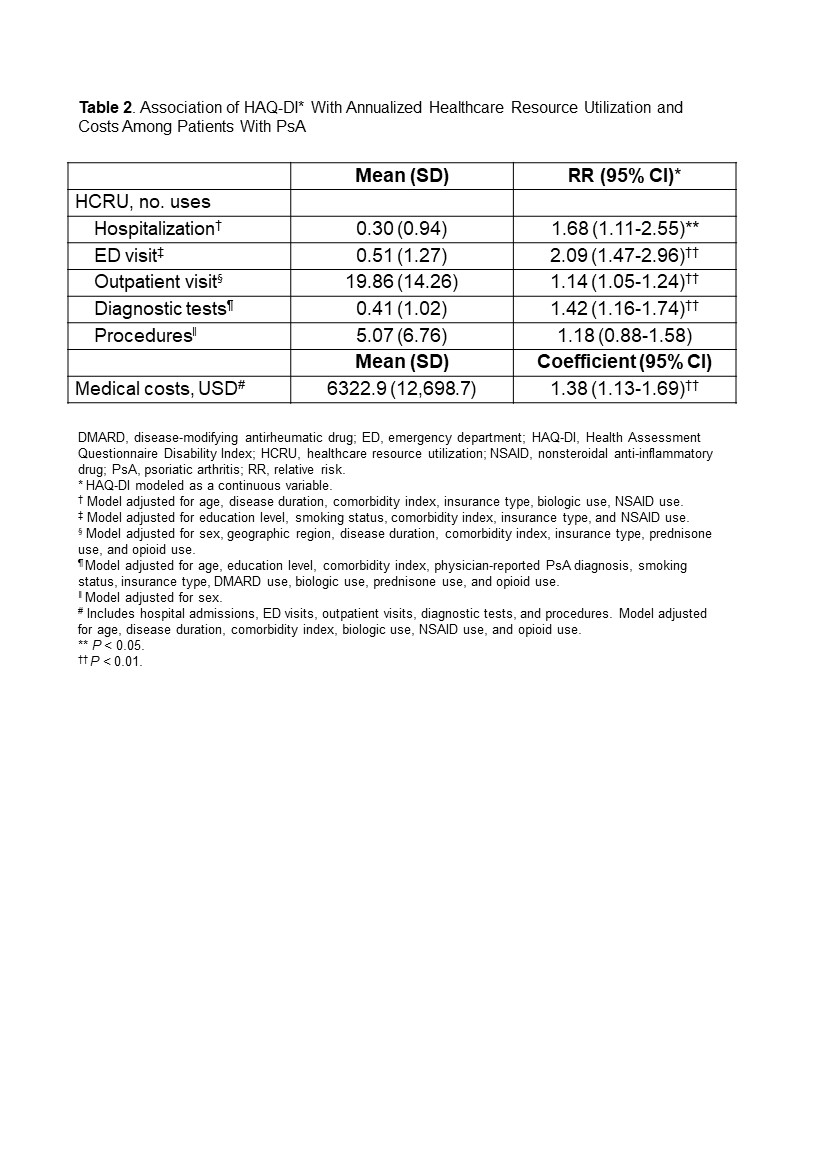
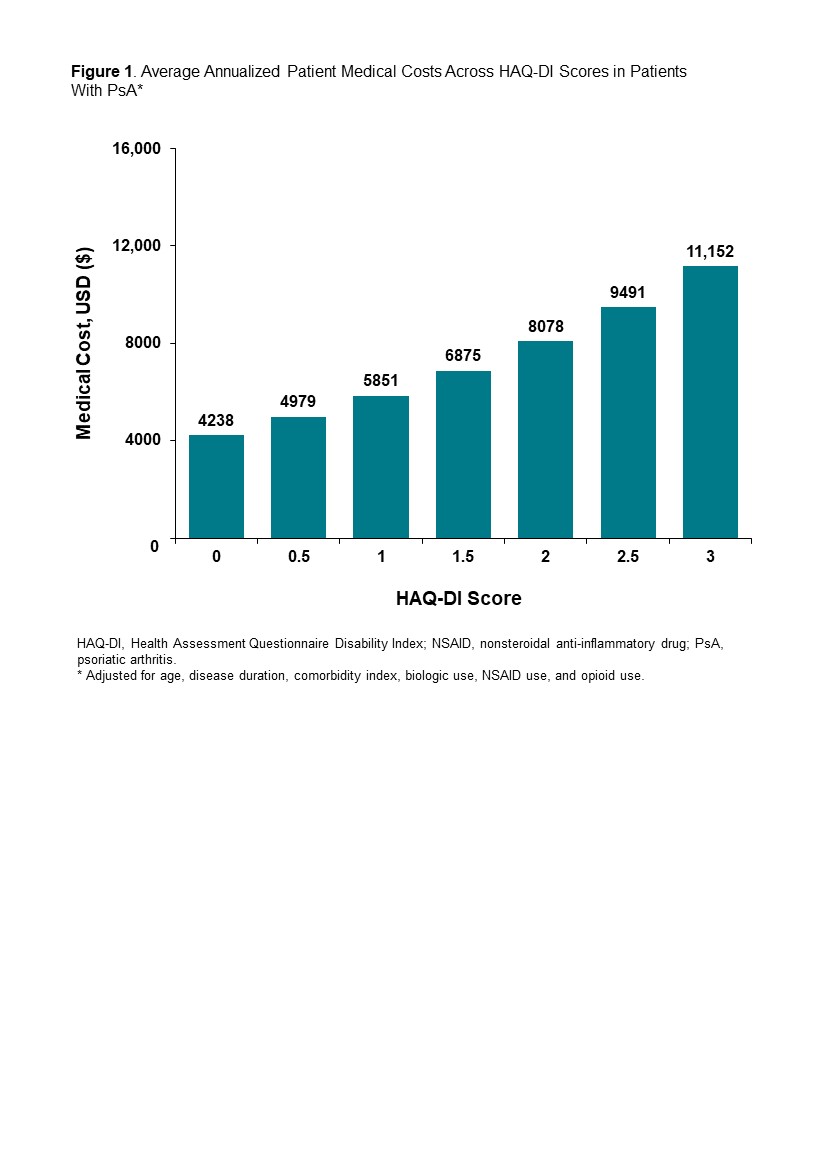
Results: A total of 828 patients with PsA who completed HAQ-DI questionnaires were included. The mean (SD) age was 58.5 (13.5) years, 72.3% were female, and 92.3% were white. The mean (SD) disease duration was 17.5 (12.4) years, and the mean (SD) HAQ-DI score at the time of the patients’ most recent questionnaire was 0.9 (0.7) (Table 1). Increasing HAQ-DI score was significantly associated with increased risk (relative risk [95% CI]) of hospitalizations (1.68 [1.11-2.55]), ED visits (2.09 [1.47-2.96]), outpatient visits (1.14 [1.05-1.24]), and diagnostic tests (1.42 [1.16-1.74]) (Table 2). There was also a significant positive association between greater HAQ-DI score and increased medical costs (coefficient [95% CI], 1.38 [1.13-1.69]) (Table 2). Overall, adjusted average patient medical costs increased with increasing HAQ-DI score (Figure 1).
Conclusion: Among patients with PsA, higher HAQ-DI scores were associated with greater HCRU and increased medical costs. These results suggest that interventions that improve functional status may reduce economic burden for patients and healthcare systems throughout the course of disease.
To cite this abstract in AMA style:
Ogdie A, Hwang M, Veeranki P, Portelli A, Sison S, Shafrin J, Pedro S, Hur P, Kim N, Michaud K. Healthcare Utilization and Costs Associated with Functional Status in Patients with Psoriatic Arthritis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/healthcare-utilization-and-costs-associated-with-functional-status-in-patients-with-psoriatic-arthritis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/healthcare-utilization-and-costs-associated-with-functional-status-in-patients-with-psoriatic-arthritis/