Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Juvenile idiopathic arthritis (JIA) and systemic lupus erythematosus (SLE) are chronic autoimmune diseases that can be complicated by significant morbidity. There are also known disparities in patients with pediatric SLE (pSLE) and JIA. Our project sought to evaluate the childhood opportunity index (COI) by race/ethnicity, language, and insurance type. Furthermore, we assessed healthcare utilization in patients with JIA and pSLE based on race, ethnicity, language, insurance, and COI by evaluating the number of acute care visits (emergency department [ED], urgent care [UC]), hospitalizations, rheumatology visits, and other outpatient specialty visits in this population.
Methods: We assessed the subset of our patients with JIA and pSLE seen between 2019 and April 2024 who have data in our population health subsidiary. This subsidiary has data from Medicaid payers and 3 commercial payers in our metro area. We collected demographic variables including race, ethnicity, and language in addition to insurance type, hospitalizations and readmissions, and emergency department, urgent care, and specialty outpatient clinic utilization. A census tract, based on each patient’s available address, was utilized to determine the national COI, which is categorized as very high (81-100), high (61-80), moderate (41-60), low (21-40), and very low (1-20). We calculated annualized rates for the number of events per 1000 patients based on utilization variables and member months.
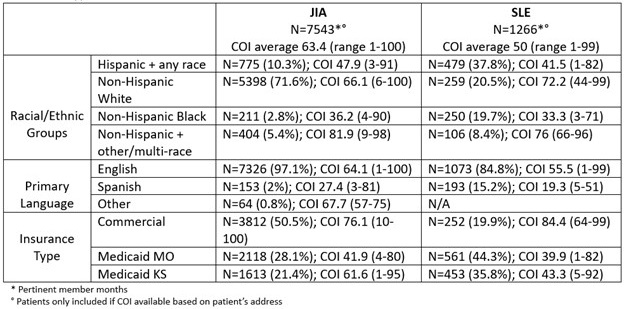
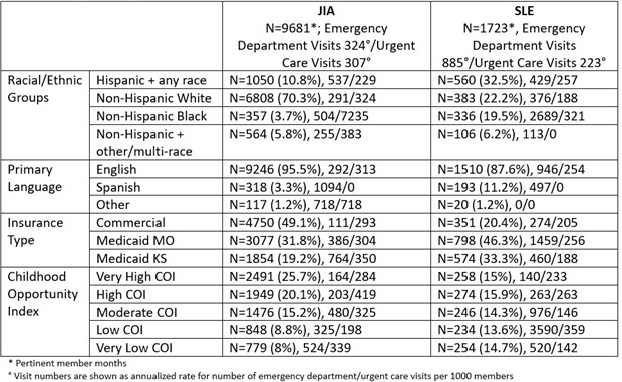
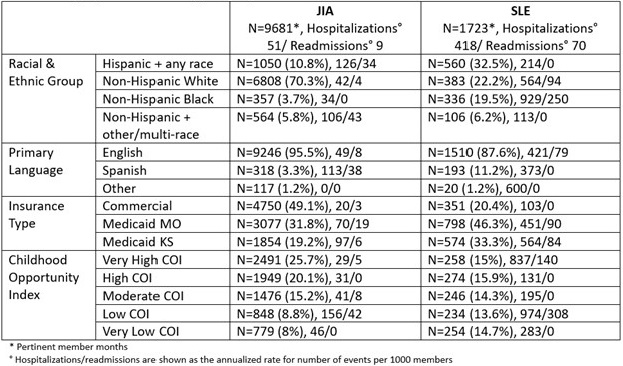
Results: We evaluated data from 1274 patients – 1087 with JIA and 187 with pSLE. The COI for patients with JIA (63.4) was in the high range compared to moderate range for patients with SLE (50) (Table 1). The COI in patients with JIA was 36.2 in Black patients and 66.1 in White patients. For SLE patients, the average COI in Black patients was 33.3, 41.5 in Hispanic patients, and 72.2 in White patients. Language led to a difference in average COI scores as well: English JIA/SLE 64.1/55.5 and Spanish JIA/SLE 27.4/19.3. Lower COIs were also noted in patients on Medicaid versus commercial insurance. Table 2 highlights higher ED utilization in Black and Hispanic patients compared to White patients in both JIA and SLE. For patients with SLE, a low COI led to over 25 times greater ED utilization rate compared to very high COI. Medicaid patients from one state with SLE are also 5 times more likely to go to the ED than patients with a commercial payer. Hospitalization rates were over 8 times higher in patients with SLE versus JIA (Table 3). Hispanic patients with JIA were 3 times more likely than White patients to be hospitalized. In SLE, both Medicaid populations were more than 4 times more likely to be hospitalized compared to patients on commercial insurance. The annualized rate per 1000 patients for rheumatology clinic visits by racial/ethnic group ranged from 2000-2560 for JIA and 2679-3572 for SLE.
Conclusion: We found disparities in healthcare utilization in patients with JIA and SLE related to race, ethnicity, language, insurance type, and COI. We plan to link our data to patient outcomes and assess for associated health disparities in addition to assessing for and addressing social determinants of health with the ultimate goal of reducing inequities and optimizing care delivery.
To cite this abstract in AMA style:
Harris J, Cooper A, Harris L. Healthcare Utilization and Childhood Opportunity Index in Patients with Juvenile Idiopathic Arthritis and Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/healthcare-utilization-and-childhood-opportunity-index-in-patients-with-juvenile-idiopathic-arthritis-and-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/healthcare-utilization-and-childhood-opportunity-index-in-patients-with-juvenile-idiopathic-arthritis-and-systemic-lupus-erythematosus/