Session Information
Session Type: Abstract Session
Session Time: 2:00PM-3:30PM
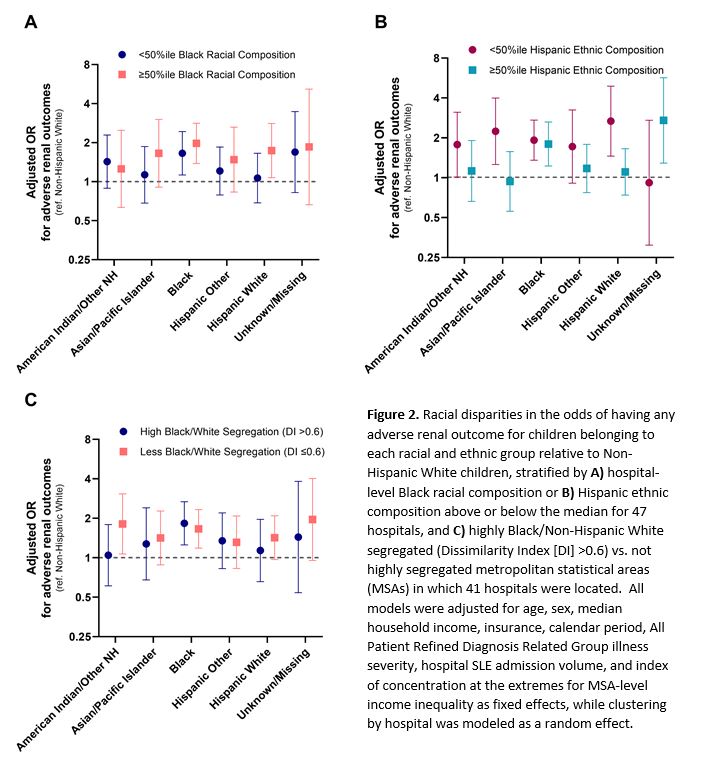
Background/Purpose: Racial disparities and hospital-level variation in pediatric SLE (pSLE) outcomes are well described, but it is not known how the racial and ethnic composition of the populations hospitals serve contributes to these disparities. Using de-identified data, we evaluated whether hospital minority composition, a measure of health care segregation, or metropolitan statistical area (MSA)-level racial or ethnic segregation modify racial disparities in pSLE outcomes.
Methods: We linked data from the Pediatric Health Information System (2006–2021) for patients 5-26 years old hospitalized for SLE to MSA-level 2020 U.S. Census and American Community Survey data. Primary outcomes assessed at the patient level were intensive care unit (ICU) stays and adverse renal outcomes (end stage renal disease, dialysis, or transplant). Hospital Black racial composition and Hispanic ethnic composition were based on % of all admissions (any indication) reported by each hospital. MSA segregation was measured by census-derived Dissimilarity Index (DI) for Black/Non-Hispanic White (NHW) or Hispanic/Non-Hispanic segregation, reflecting evenness of spatial distribution of two groups across census tracts within an MSA. We compared indices using mixed effects logistic models with hospital-level random effects, adjusted for calendar period, sociodemographics, severity indicators, and hospital volume. We stratified hospitals by above or below the median for Black or Hispanic composition and by high or low Black/NHW segregation.
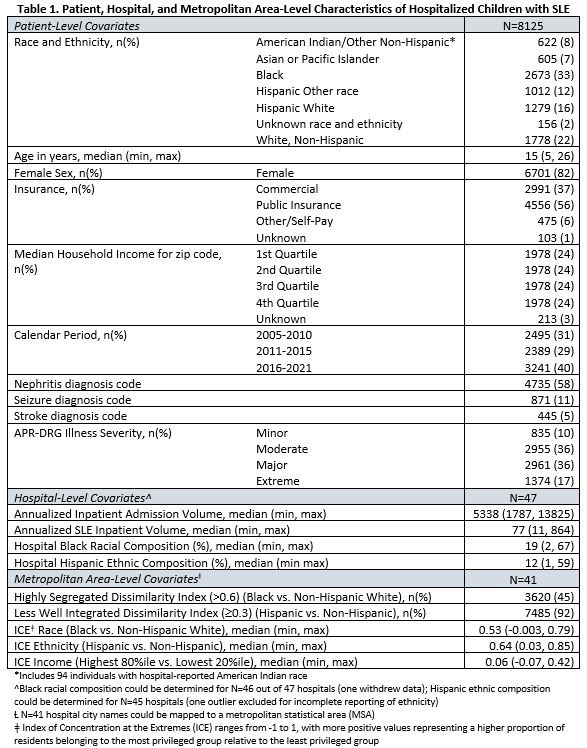
Results: Of 8125 patients (at 47 hospitals), 2293 (28%) ever required ICU care and 698 (9%) had an adverse renal outcome (Table 1). Higher hospital Hispanic composition, but not Black racial composition, associated with lower overall odds of ICU stay (OR 0.99 [0.986-0.996] per % increase). Significant Black vs. NHW disparity in ICU care was observed only at hospitals with high Black racial composition, whereas Hispanic vs. NHW disparities in ICU stay did not differ by hospital Hispanic composition (Fig 1).
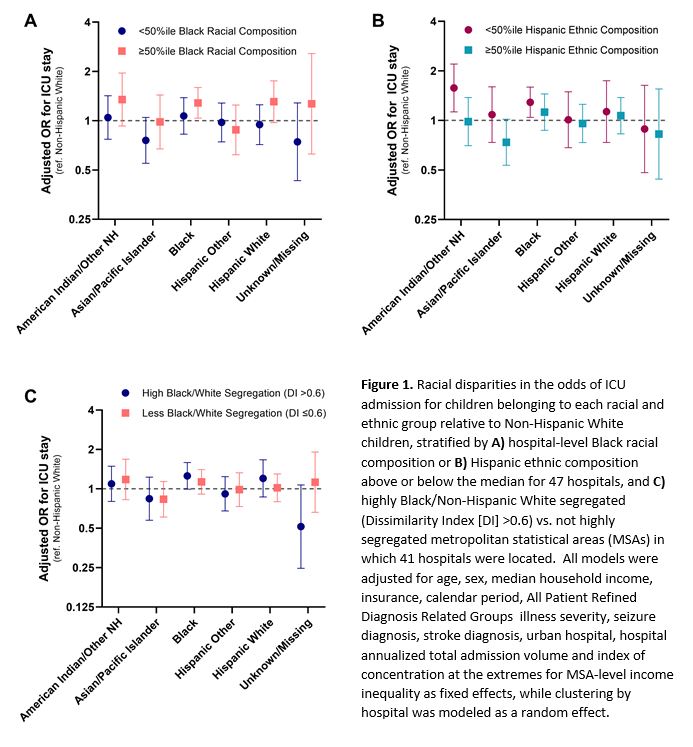
Similarly, the magnitude of Black vs. NHW disparity in renal outcomes was larger at hospitals with high Black racial composition (OR 2.0 [1.4-2.8] vs. 1.7 [1.1-2.4]). Moreover, disparities in renal outcomes for Hispanic White vs. NHW children were only observed at hospitals with high Black racial composition (Fig 2A). We observed the opposite for Hispanic composition, where Hispanic White, Asian, and American Indian/Other vs. NHW disparities were only apparent at hospitals with low Hispanic composition (Fig 2B).
MSA-level DI was not significantly associated with either outcome. Black vs. NHW disparities did not differ by high (DI >0.6) vs. low MSA Black/NHW segregation (Fig 1C, 2C). No MSAs met criteria for high Hispanic/Non-Hispanic segregation.
Conclusion: Racial disparities in pSLE outcomes are magnified at hospitals serving a greater proportion of Black patients, which may reflect negative effects of health care segregation and inequitable hospital resources. Metropolitan level measures of segregation explain little variance in hospital outcomes, therefore linkages to small geographic units must be included in health care databases to understand local factors that contribute to poor outcomes.
To cite this abstract in AMA style:
Chang J, Liu J, Berbert L, Weller E, Alonzi G, Smitherman E, Patel P, Son M, Costenbader K. Health Care Segregation, but Not Metropolitan Area Segregation, Magnifies Racial Disparities in Hospital Outcomes of Pediatric Lupus [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/health-care-segregation-but-not-metropolitan-area-segregation-magnifies-racial-disparities-in-hospital-outcomes-of-pediatric-lupus/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/health-care-segregation-but-not-metropolitan-area-segregation-magnifies-racial-disparities-in-hospital-outcomes-of-pediatric-lupus/