Session Information
Date: Monday, November 14, 2022
Title: SLE – Diagnosis, Manifestations, and Outcomes Poster III: Outcomes
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: While long-term follow-up (FU) is needed to unmask poor outcome in lupus nephritis (LN), most clinical trials evaluate outcome measures at short-term. Early endpoints predictive of long-term outcome in LN are therefore most welcome to compare efficacy of pharmacological interventions. A multicentric study, using a large database of prospectively followed LN patients, succeeded in computing equations (hazard index; HI) predicting adverse kidney outcomes, i.e. chronic kidney disease (CKD), severe kidney injury (SKI) and renal replacement therapy (RRT). These HI were calculated with data measured within the first year of treatment. The HI values were significantly higher in patients experiencing long-term poor renal outcomes after 4 years of follow-up (FU) (Mackay M et al. Arthritis Rheumatol 2016; 68 (suppl.10), abstract 967). We confirmed the validity of the HI equations in an independent cohort (Tamirou F et al. Arthritis Rheumatol 2018; 70 (suppl.10), abstract 1945). The initial HI equations were revised in a subsequent analysis (Mackay M et al. Arthritis Rheumatol 2019;71;411-419), taking into account additional baseline data.
To validate the revised HI for CKD, SKI and RRT in the Louvain LN cohort followed for ≥ 4 years and to check their validity to predict RTT in patients followed for a longer period.
Methods: Data from 262 consecutive LN patients followed in our lupus center were screened. Only those for whom clinical data were available following their first episode of proliferative and/or membranous biopsy-confirmed LN were selected. Serum creatinine and proteinuria at different time points from 131 LN patients followed for ≥ 4 years were analyzed. At last FU, patients were divided according to the presence or absence of CKD, SKI and RRT. Their respective HI, measured at one year, were compared. CKD/SKI were defined as ≥ 30%/≥ 50% decrease in eGFR (CKD-EPI equation), compared to the highest value measured within the first year.
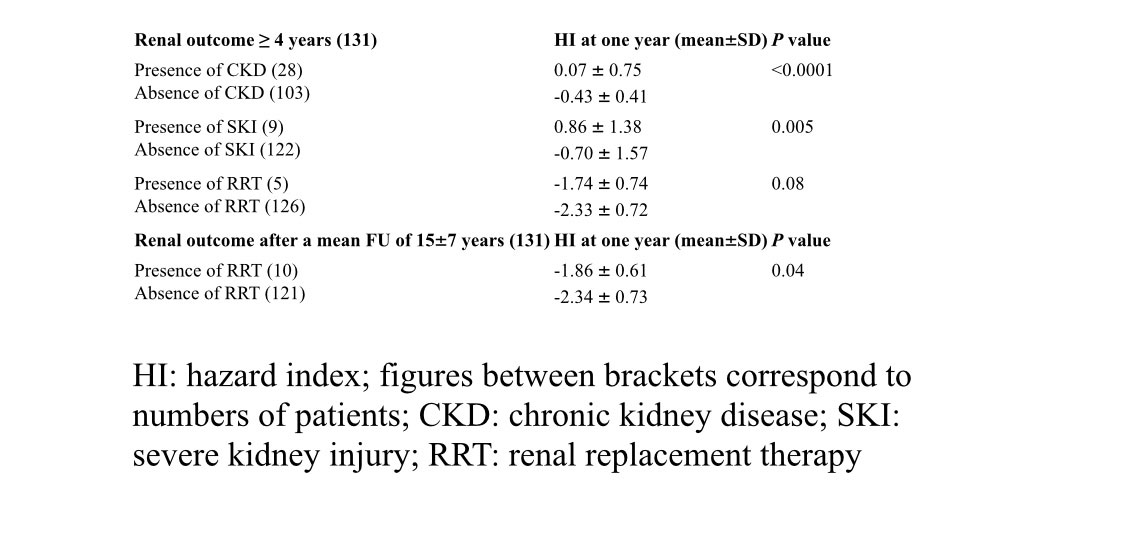
Results: As illustrated in the Table, the mean HI for CKD and SKI, measured at one year, were significantly higher in the groups of patients who indeed developed CKD and SKI after a FU of ≥ 4 years compared to those who did not. The mean HI for RRT was higher in patients who developed RRT after ≥ 4 years but the difference was not statistically significant (p=0.07), most likely due to the small numbers of RRT in this series at this time-point (n=5). After a longer FU (mean ± SD: 15 ± 7 years), more RRT were observed (n=10) and the mean HI for RRT became significantly higher in patients suffering from RRT compared to those who did not. Of note, clinical (gender, age, mean serum creatinine, mean serum creatinine, mean proteinuria) and pathological (ISN/RPS class) characteristics did not differ at baseline between patients with poor long-term renal outcome compared to the others.
Conclusion: We confirm the validity of the revised HI equations as early predictors of poor renal outcomes in a cohort of incident LN, including for RRT. These HI tools could be proposed as outcome measures in LN clinical trials.
To cite this abstract in AMA style:
Tamirou F, Houssiau F. Hazard Index Equations Using Data Collected at Baseline and After One Year Treatment Allow Early Prediction of Poor Outcome in an Incident Lupus Nephritis Population: Data from the Louvain Lupus Nephritis Cohort [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/hazard-index-equations-using-data-collected-at-baseline-and-after-one-year-treatment-allow-early-prediction-of-poor-outcome-in-an-incident-lupus-nephritis-population-data-from-the-louvain-lupus-nephr/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/hazard-index-equations-using-data-collected-at-baseline-and-after-one-year-treatment-allow-early-prediction-of-poor-outcome-in-an-incident-lupus-nephritis-population-data-from-the-louvain-lupus-nephr/