Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Systemic lupus erythematosus (SLE) is a complex chronic autoimmune disease of unknown etiology. Previous studies of beauty products as potential triggers of SLE development have shown conflicting results. Our study evaluates the use of hair chemicals in patients with SLE and controls and the relationship of use with disease severity among patients.
Methods: Data was obtained from an ongoing longitudinal registry of patients with SLE and non-SLE population-matched controls at a single center. Participants seen over a 12 year period. Information on demographics, medical history, social history, types of hair chemicals used, and SLE characteristics (if applicable) was gathered from in-person interviews. Chart review and telephone follow-up was done for missing values. Disease damage was determined by SLICC/ACR Damage Index (“damage present” if score ≥1). Males and children were excluded from the study population. “Cutaneous lupus” includes SLE patients with documented malar rash, discoid rash, photosensitivity, and/or alopecia. Pearson’s chi-squared testing was performed for categorical measures and two-sample t-tests were performed for continuous measures. Significance was set at alpha = 0.05.
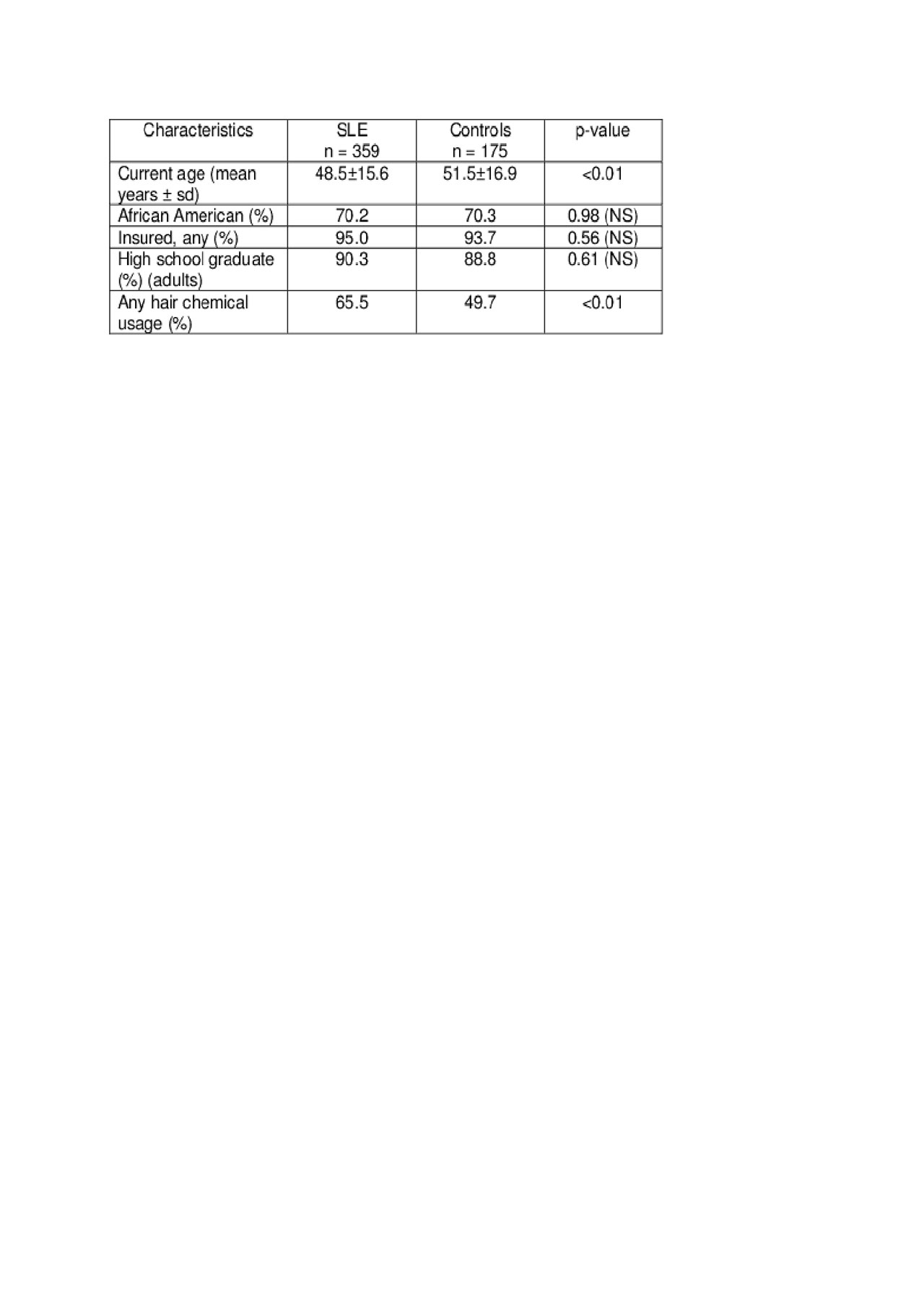
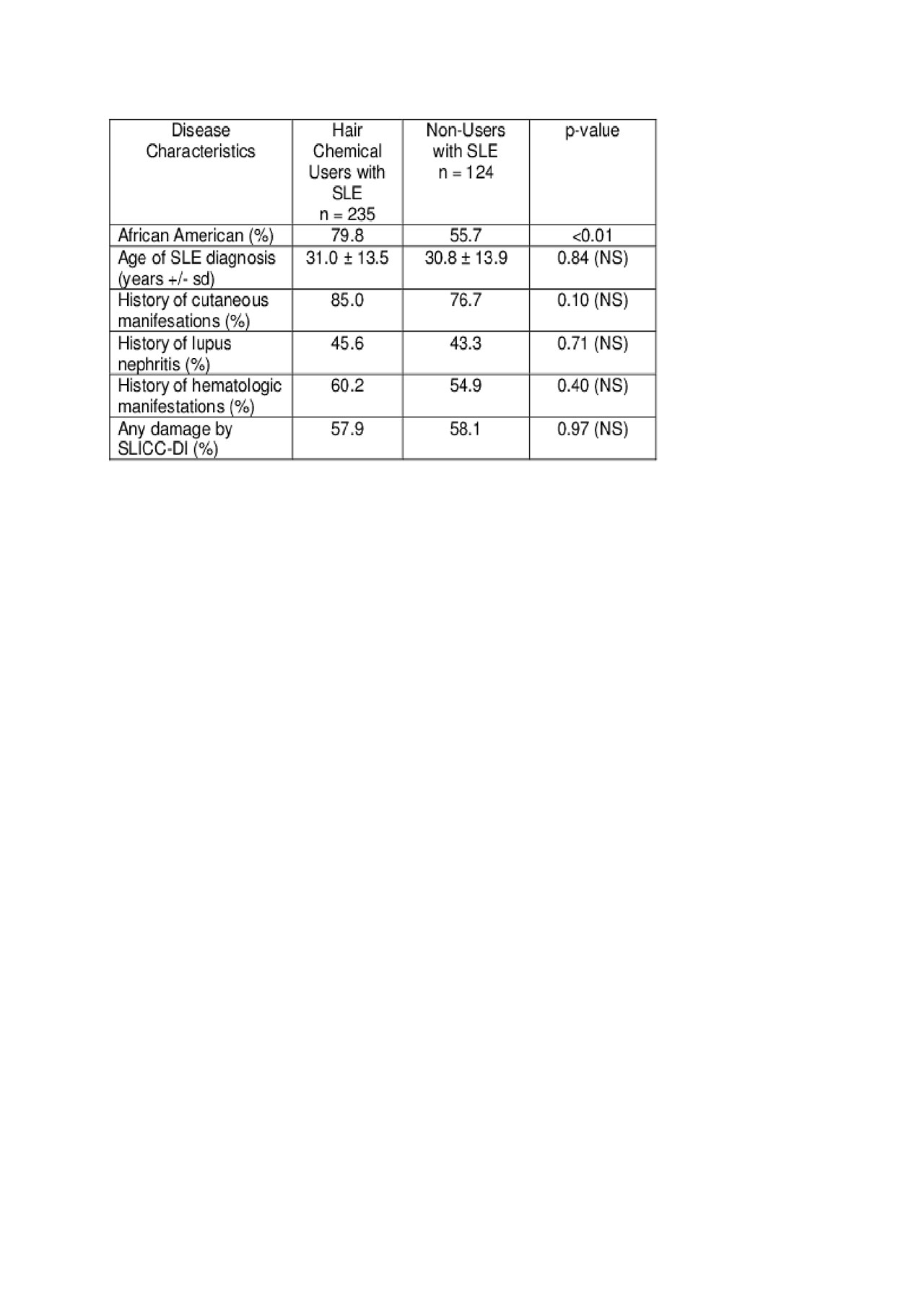
Results: A total of 359 female SLE patients and 175 female controls were included, Table 1. Hair chemical use was more frequent in self-identified black patients (p< 0.01). Patients with SLE were significantly more likely to use hair chemicals compared to controls (65.5% vs. 49.7%, p< 0.01), specifically with higher proportions of patients using hair relaxers/straighteners (p=0.91), hair dyes (p=0.07), and permanent wave products (p=0.23). SLE damage did not differ among patients who use hair chemicals compared to non-users (p=0.97), Table 2. A higher percentage of hair chemical users had cutaneous manifestations, but was not statistically significant (p=0.10)
Conclusion: In conclusion, we found that hair chemical use among females was significantly higher in patients with SLE compared to controls, especially hair dyes. These results provide a basis to look further in to hair chemical use and its relation to autoimmunity. Ongoing analyses are examining the timing and duration of hair chemical use and the development of autoimmunity.
To cite this abstract in AMA style:
English J, Faith T, Wilson D, Kamen D. Hair Chemicals and Systemic Lupus Erythematosus: A Case-Control Study [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/hair-chemicals-and-systemic-lupus-erythematosus-a-case-control-study/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/hair-chemicals-and-systemic-lupus-erythematosus-a-case-control-study/