Session Information
Date: Sunday, November 8, 2020
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Multiple studies have confirmed that the gut and stool microbiome in ankylosing spondylitis (AS) and inflammatory bowel disease (IBD) are distinct from healthy controls, and it is known that ~60% of AS cases have subclinical IBD, and 5-10% have clinical IBD. As different microbiome studies of these diseases have used different sequencing and analytic methods, it has not been possible to determine if these diseases have similar or different gut microbiomes. This study aimed to test the hypothesis that the gut microbiome in AS and IBD is different, and whether the gut microbiome in AS correlated with disease activity.
Methods: After ethics approval and written informed consent, stool samples, terminal ileal biopsies, colonic biopsies and/or rectal biopsies were obtained from 192 AS patients (136 Swedish, 33 Australian (5 with concomitant IBD, ‘AS-IBD’) and 23 Italian), 59 Australian IBD patients, and 112 controls undergoing colon cancer screening studies but with no ill-health (105 Australian and 7 Italian). Metagenomic profiling was performed using 16S rRNA sequencing and processed using Qiime2. Alpha-diversity, beta-diversity and taxonomic comparisons were controlled for age, BMI, country of origin, BMI, smoking status, gender, and TNF-inhibitor usage.
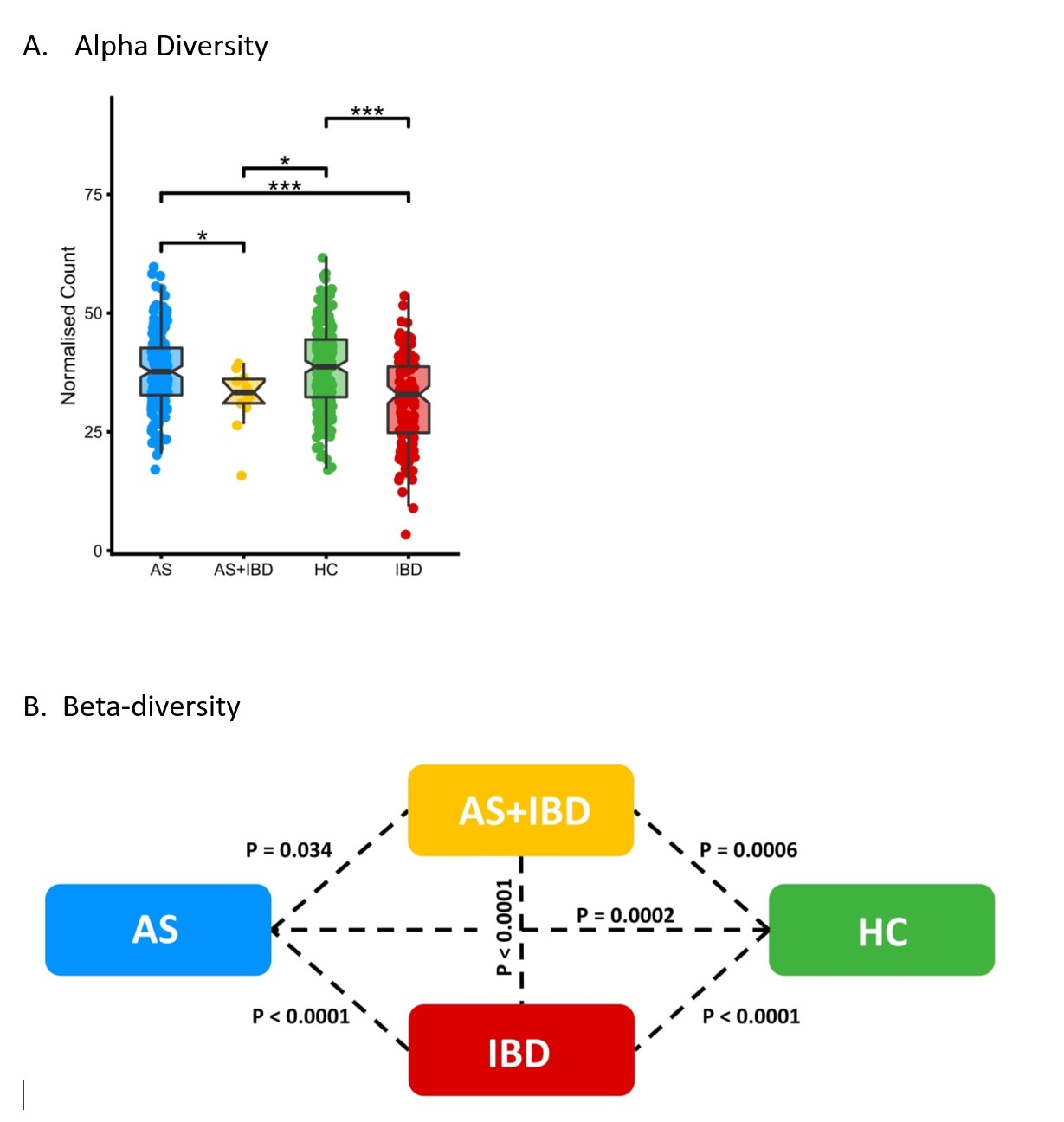
Results: AS, AS-IBD and IBD patients differed from one another and from healthy controls in both alpha and beta-diversity (Figure 1). Considering patients with either fecal calprotectin (FCP)< 100 or >100, AS patients differed in both alpha and beta-diversity from IBD patients (P< 0.01 all comparisons). FCP >100 was also associated with microbiome differentiation in AS and IBD patients. AS patients with and without clinical IBD could be distinguished from one another with moderate accuracy using stool microbiome (AUC=0.754), similar to the performance of FCP (AUC=0.752) and better than the Dudley Inflammatory Bowel Symptom Questionnaire (AUC=0.716). Stool microbiome also accurately distinguished IBD patients from healthy controls (AUC=0.757). Amongst AS patients, beta- but not alpha-diversity differed between those with BASDAI 0-2.5, 2.5-5.0, 5.0-7.5 and 7.5-10 (P=0.015). TNFi usage was associated with differentiation of the gut microbiome in IBD patients. Increased Haemophilus carriage was observed in AS, AS-IBD, AS patients with elevated BASDAI (7.5+), and IBD patients with FCP >100. Apart from Streptococcus and Haemophilus, no other indicator taxa were shared between AS and IBD patients.
Conclusion: AS and AS-IBD patients have a distinct gut microbiome compared with IBD patients and healthy controls. This is consistent with immunological and genetic evidence suggesting that the gut plays a different role in driving AS compared with IBD. AS and IBD disease activity is associated with changes in the gut microbiome.
 Comparison of Australian, Swedish and Italian AS patients, Australian IBD patients, and Australian and Italian healthy controls sampled from four body sites: terminal ileum, right colon, rectum, and stool.
Comparison of Australian, Swedish and Italian AS patients, Australian IBD patients, and Australian and Italian healthy controls sampled from four body sites: terminal ileum, right colon, rectum, and stool.
To cite this abstract in AMA style:
Sternes P, Brett L, Phipps J, Ciccia F, de Guzman E, Morrison M, Holtmann G, Klingberg E, McIvor C, Forsblad-d'Elia H, Brown M. Gut Microbiome Changes Are Different Between Ankylosing Spondylitis and Inflammatory Bowel Disease, and Correlate with Disease Activity in Both Diseases [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/gut-microbiome-changes-are-different-between-ankylosing-spondylitis-and-inflammatory-bowel-disease-and-correlate-with-disease-activity-in-both-diseases/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/gut-microbiome-changes-are-different-between-ankylosing-spondylitis-and-inflammatory-bowel-disease-and-correlate-with-disease-activity-in-both-diseases/
