Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Spinal gout is reported as a rare event, presenting as acute back pain, neuropathy, and spinal compression. Diagnosis is commonly based on identification of a mass, followed by tissue confirmation of monosodium urate (MSU) deposition. It is likely that many more cases of gout involve the spine asymptomatically or with non-specific or under-recognized symptoms.
Methods: Using dual-energy CT (DECT), we are determining the prevalence/extent of MSU deposition in the lumbosacral spines of patients with gout vs without gout, and with tophaceous vs non-tophaceous gout. We are recruiting 25 controls, 25 non-tophaceous and 25 tophaceous gout patients, 50-80 years old. Exclusion criteria include known CPPD disease, RA, spondyloarthropathy or active spinal malignancy. All gout subjects meet ACR classification criteria and have entry serum urate (sU) of >6.8 mg/dL, or sU >6.0 mg/dL on ULT for < 6 months. Demographics, gout history, Aberdeen back pain scale, sU, ESR, and CRP are collected. Subjects undergo DECT of the lumbosacral spine to assess for MSU deposition and osteoarthritic changes.
Results: 61 subjects are enrolled to date (25 control, 24 non-tophaceous and 12 tophaceous gout). Control and gout (all pooled) subjects have similar mean age in years (controls, 61.8±3.8 vs gout, 64.1±7.32, p=0.15), but differ in BMI (controls, 28.3±6.5 kg/m2 vs gout, 32.35±6.9 kg/m2, p=0.02) and creatinine (controls, 1.0±0.2 mg/dL vs gout, 1.5±0.7 mg/dL, p< 0.05). Mean sU and ESR are higher in gout subjects (sU-controls, 5.3±1 mg/dL vs gout, 8.7±1.7 mg/dL, p< 0.05; ESR-controls, 13.7±13.8 mm/h vs gout, 25.3±18.3 mm/h, p< 0.05). Using default threshold settings for MSU visualization, greater MSU deposition is observed in the spine of gout patients (controls, 2.2±1.2 cm3 vs gout, 10.8±32.2 cm3, p=0.18; Fig 1). When a single gout outlier with excessively high sU and spinal MSU is excluded, spinal MSU deposition between controls and gout patients becomes significant (controls, 2.2±1.2 cm3 vs gout, 5.6±7.8 cm3, p=0.04). Reanalysis of several scans using narrower threshold settings to limit possible artifact confirms increased MSU signal among gout patients. Although many subjects in each group do not have excessive MSU deposition, deposition is more common in both gout groups (Fig 2). Thus far, MSU deposition is not different between non-tophaceous and tophaceous gout patients (non-tophaceous, 12.3±2.92 cm3 vs tophaceous, 7.9±3.2 cm3, p = 0.7). No subject demonstrated a frank spinal tophus. Gout patients report higher back pain scores (controls, 5.7±8.3, vs gout, 11.8±14.3, p=0.06). Across all groups deposition is greater in patients with higher sU.
Conclusion: Based on preliminary results, gout patients have higher inflammatory markers, more spinal MSU deposition, and increased back pain versus controls. Preliminary results with more stringent DECT threshold settings suggests these differences are not artifact, but analysis is ongoing. These data suggest that non-tophaceous MSU deposition in the spine occurs in a subset of gout patients, is associated with sU level, and may be associated with low back pain.
Supported by an investigator-initiated grant from Horizon Therapeutics.
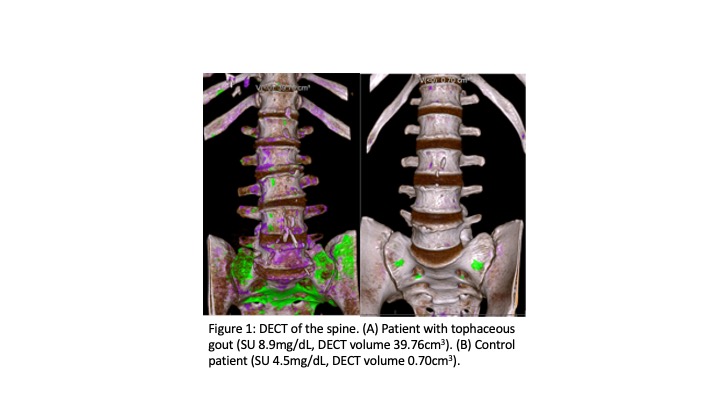 Figure 1: DECT of the spine. (A) Patient with tophaceous gout (SU 8.9mg/dL, DECT volume 39.76cm3). (B) Control patient (SU 4.5mg/dL, DECT volume 0.70cm3).
Figure 1: DECT of the spine. (A) Patient with tophaceous gout (SU 8.9mg/dL, DECT volume 39.76cm3). (B) Control patient (SU 4.5mg/dL, DECT volume 0.70cm3).
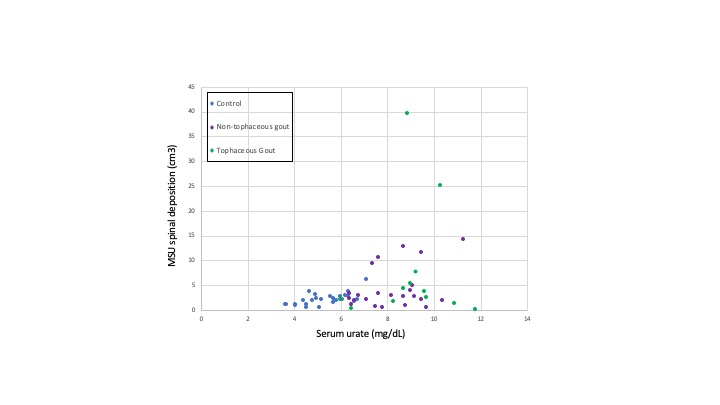 Figure 2: SU versus MSU spine deposition in control and gout patients
Figure 2: SU versus MSU spine deposition in control and gout patients
To cite this abstract in AMA style:
Toprover M, Mechlin M, Slobodnick A, Pike V, Oh C, Davis C, Fields T, Becce F, Pillinger M. Gout and Serum Urate Levels Are Associated with Lumbar Spine Monosodium Urate Deposition and Chronic Low Back Pain: A Dual-Energy CT Study [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/gout-and-serum-urate-levels-are-associated-with-lumbar-spine-monosodium-urate-deposition-and-chronic-low-back-pain-a-dual-energy-ct-study-2/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/gout-and-serum-urate-levels-are-associated-with-lumbar-spine-monosodium-urate-deposition-and-chronic-low-back-pain-a-dual-energy-ct-study-2/
