Session Information
Date: Monday, November 14, 2022
Title: Abstracts: RA – Diagnosis, Manifestations, and Outcomes III: RA ILD
Session Type: Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: RA-associated interstitial lung disease (RA-ILD) is an extra-articular manifestation of RA causing substantial morbidity and mortality. Genetic risk variants, such as the MUC5B rs35705950 promoter variant, have been linked to both idiopathic pulmonary fibrosis and RA-ILD. The purpose of this study was to validate these findings in a large RA cohort and to evaluate for the presence of racial differences, gene-smoking, and gene-disease activity interactions in RA-ILD risk, which have not been previously examined.
Methods: Participants were enrollees in a multicenter prospective cohort of U.S. Veterans with RA who underwent genotyping using the Infinium Global Screening Array-24 v2.0 microarray. Single nucleotide polymorphisms (SNP) for MUC5B rs35705950 and TOLLIP rs5743890 were examined assuming autosomal dominant inheritance. Genotyping was separately performed for HLA-DRB1 shared epitope (SE) alleles. ILD diagnoses were validated through systematic medical record review, with all ILD patterns included. Gene associations with ILD were assessed using logistic regression in the overall cohort and then stratified by self-reported race, smoking status, and mean disease activity over follow-up (DAS28 ≤ or >3.2). Gene interactions with race, smoking, and DAS28 were assessed by calculating the relative excess risk of interaction (RERI).
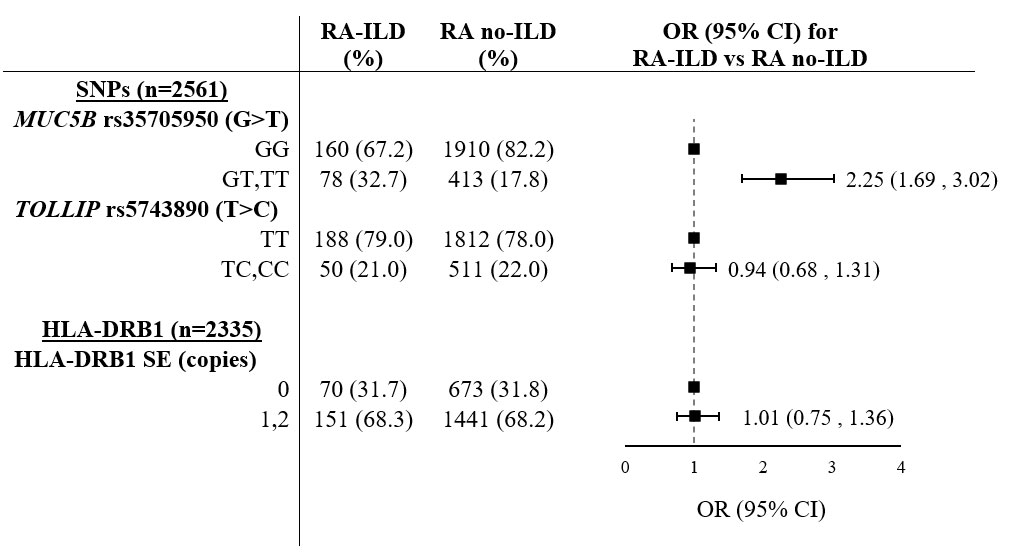
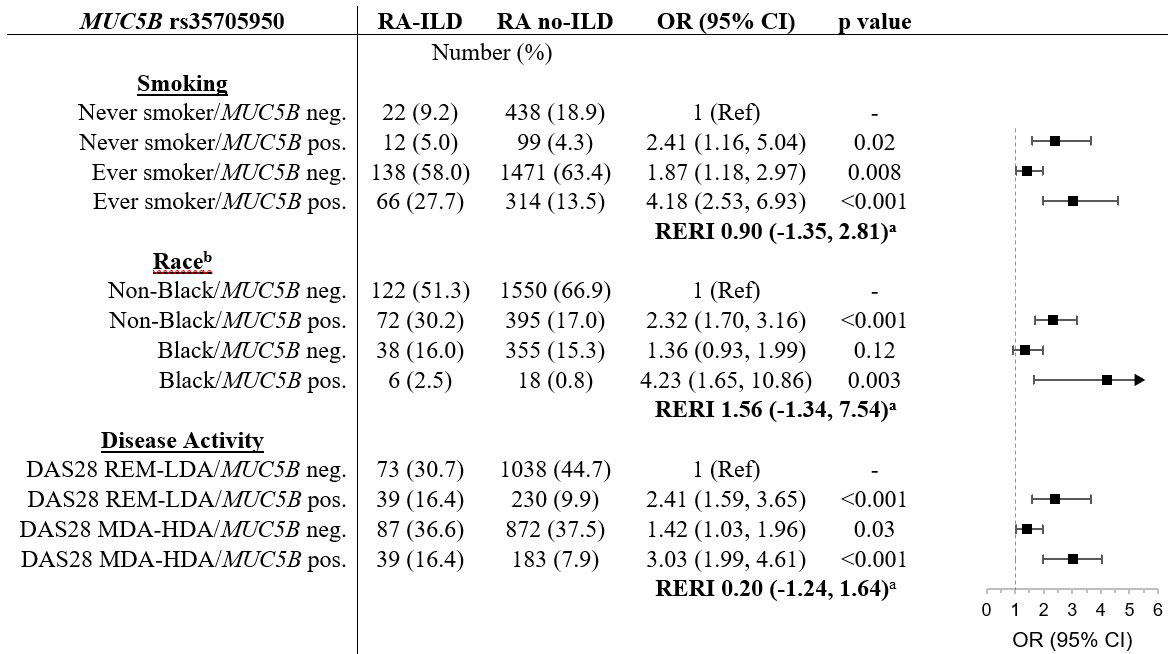
Results: We studied 2,561 participants (89% male, 77% White, 16% Black/African American), with 238 (9.3%) having ILD. The MUC5B variant was associated with ILD (OR 2.25 [95% CI 1.69-3.02]; Table 1), whereas the TOLLIP variant and HLA-DRB1 SE were not. The MUC5B variant was only associated with ILD in a usual interstitial pneumonia (UIP) pattern (OR 3.09 [95% CI 1.89, 5.04). While the MUC5B variant was less frequent in Black/African American participants (5.8%) than the remainder of the cohort (21.8%), the odds of RA-ILD among Black/African American participants with the MUC5B variant was similar (OR 4.23 [1.65, 10.86] vs. OR 2.32 [1.70, 3.16]), without a significant additive interaction (RERI 1.56 [-1.34, 7.54])(Table 2). MUC5B and ILD associations were numerically higher among smokers than non-smokers (OR 4.18 [2.53, 6.93] vs. OR 2.41 [1.16, 5.04]), but there was no significant additive interaction (RERI 0.90 [-1.35, 2.81]). MUC5B and ILD associations were similar in the remission/low disease activity (OR 2.41 [1.59, 3.65]) and moderate/high disease activity groups (OR 3.03 [1.99, 4.61]), with no additive interaction (RERI -0.20 [-1.24, 1.64]). There were no differences in ILD risk attributable to either the TOLLIP variant or HLA-DRB1 SE based on race, smoking status, or disease activity (not shown).
Conclusion: In this large RA cohort, the MUC5B promoter variant was associated with >2-fold higher odds of RA-ILD. While this genetic variant is less common among the Black/African American population, it appears to portend risk of ILD at least as strong as in other racial groups. No significant additive interactions were detected between MUC5B and race, smoking, or disease activity. These findings support the development of precision risk models for RA-ILD to enable early identification and ultimately prevention.
Abbreviations: ILD (interstitial lung disease), OR (odds ratio), SE (shared epitope)
Abbreviations: ILD (interstitial lung disease), RA (rheumatoid arthritis), OR (odds ratio), RERI (relative excess risk of interaction), REM-LDA (remission or low disease activity), MDA-HAD (moderate or high disease activity), CI (confidence interval)
a: RERI is represented as relative risk with 95% confidence interval.
b: Black represents individuals reporting Black/African American race. Non-Black represents individuals reports White, Asian American, American Indian/Pacific Islander, other, or unknown.
To cite this abstract in AMA style:
Wheeler A, Yang Y, Baker J, Poole J, Ascherman D, Kerr G, Reimold A, Kunkel G, Cannon G, Wysham K, Singh N, Lazaro D, Monach P, Bridges, Jr. S, Mikuls T, England B. Genetic and Environmental Risk Factors in Rheumatoid Arthritis-Associated Interstitial Lung Disease [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/genetic-and-environmental-risk-factors-in-rheumatoid-arthritis-associated-interstitial-lung-disease/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/genetic-and-environmental-risk-factors-in-rheumatoid-arthritis-associated-interstitial-lung-disease/