Session Information
Date: Sunday, October 26, 2025
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: To apply current treatment recommendations for psoriatic arthritis (PsA), clinicians must perform a comprehensive assessment of psoriatic disease domains, including a musculoskeletal exam (tender and swollen joints, dactylitis, enthesitis, axial disease) and a skin and nail exam for psoriasis (PsO). Documentation in the electronic medical record (EMR) serves as a proxy for these assessments. Additionally, ICD coding of psoriatic disease influences administrative database research. This study aimed to compare documentation of psoriatic domains and ICD coding practices between PsA specialist providers and general rheumatologists at two academic centers.
Methods: We identified patients with ICD-coded diagnoses of PsA who were seen by either general rheumatologists or PsA combined-clinic specialist providers at two established PPACMAN (Psoriasis and Psoriatic Arthritis Clinics Multicenter Advancement Network) sites. Clinical notes were reviewed for documentation of musculoskeletal and cutaneous PsA domains. We also evaluated the accuracy and completeness of ICD coding for PsA and/or PsO to assess the reliability of EMR-derived discrete data. Fisher’s exact tests were used to assess relationships between provider type, documentation practices, and ICD coding.
Results: Across multiple academic centers, PsA combined-clinic specialist providers documented psoriatic disease domains significantly more consistently than general rheumatologists. Musculoskeletal domains—including tender and swollen joint counts (p< 0.001), assessment of spondyloarthritis (p=0.017), dactylitis (p< 0.001), and enthesitis (p< 0.001)—were more routinely documented by PsA specialists. Cutaneous domains were also more consistently documented by specialists, including PsO location (p< 0.001), phenotypic subset (p< 0.001), and use of standardized psoriasis assessment tools such as BSA, PGA, and PASI scores (p< 0.001). Furthermore, PsA specialists more frequently applied appropriate ICD codes for PsO (p< 0.001) and for both PsA and PsO (p< 0.001).
Conclusion: In this multicenter retrospective study, PsA specialist providers more thoroughly documented musculoskeletal and cutaneous disease domains and more accurately coded for PsA and PsO compared to generalists. These findings highlight gaps in documentation among general rheumatologists and underscore the need for enhanced training in psoriatic disease assessment. Despite significant efforts from multiple organizations, patient advocacy foundations and academics to increase awareness, improvement in both assessment and documentation are still needed. Improved documentation tools may facilitate both better clinical evaluation and more reliable research using EHR or claims-based data.
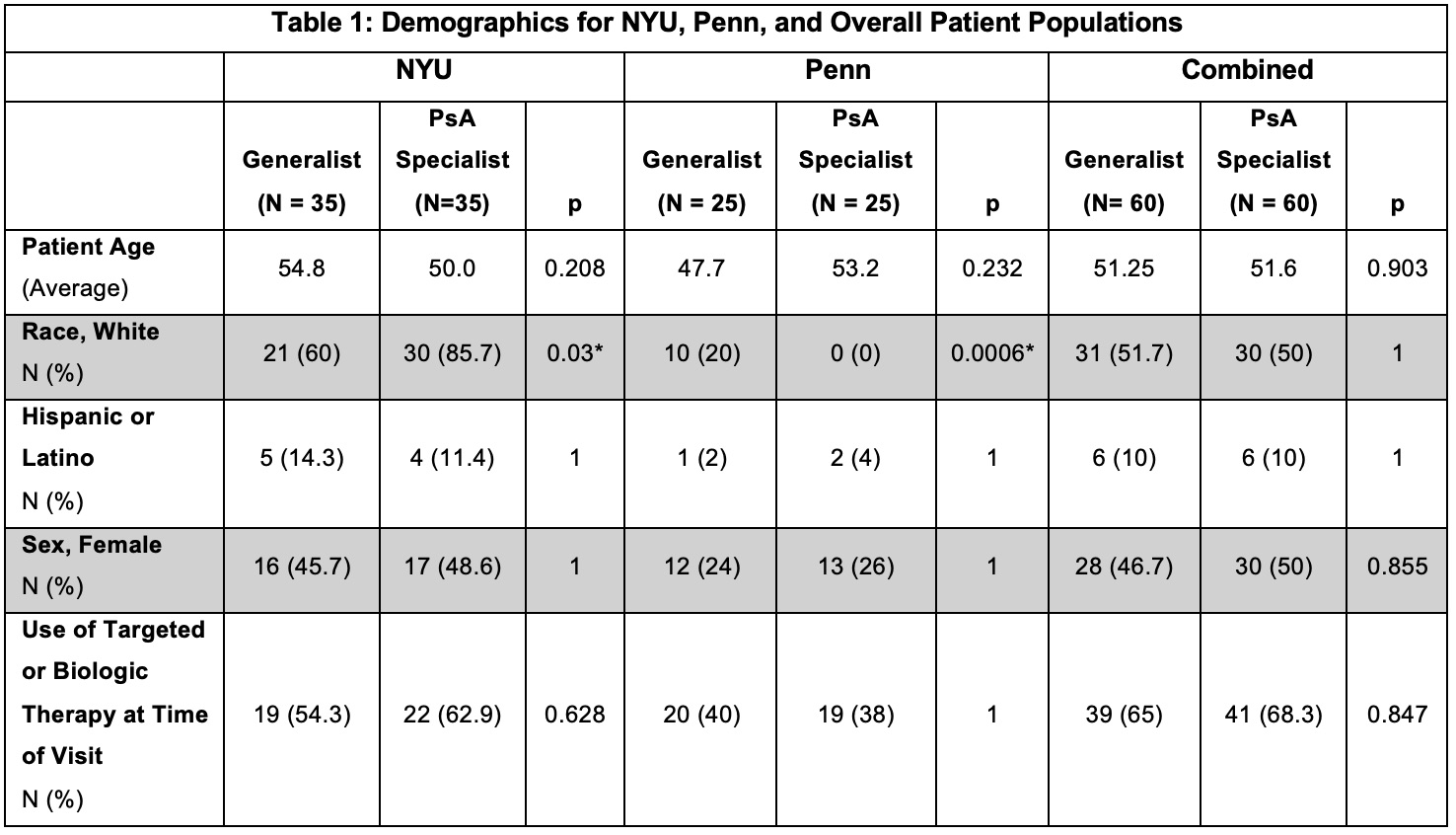 Table 1: Demographics for NYU, Penn, and Combined Patient Populations, grouped by provider type and institution
Table 1: Demographics for NYU, Penn, and Combined Patient Populations, grouped by provider type and institution
.jpg) Table 2: Documentation of Psoriatic Disease Domains, grouped by provider type and institution
Table 2: Documentation of Psoriatic Disease Domains, grouped by provider type and institution
.jpg) Table 3: Documentation of ICD Coded Diagnoses, grouped by provider type and institution
Table 3: Documentation of ICD Coded Diagnoses, grouped by provider type and institution
To cite this abstract in AMA style:
Rice A, Hopkins Gillespie S, Sai N, Reddy S, Merola J, Haberman R, Ogdie A, Scher J. Gaps In Documentation Of Psoriatic Arthritis Domains In General Rheumatologic Practices Compared To Rheumatology-Dermatology Combined Clinics [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/gaps-in-documentation-of-psoriatic-arthritis-domains-in-general-rheumatologic-practices-compared-to-rheumatology-dermatology-combined-clinics/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/gaps-in-documentation-of-psoriatic-arthritis-domains-in-general-rheumatologic-practices-compared-to-rheumatology-dermatology-combined-clinics/
