Session Information
Date: Monday, November 13, 2023
Title: (1264–1307) RA – Diagnosis, Manifestations, and Outcomes Poster II
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: With the advent of new therapies and increasing life expectancy, there is a rising number of older adults living with rheumatoid arthritis (RA). Patients with RA are at a higher risk for developing frailty1, and frailty in RA has been linked with increased risk of hospitalization2. However, little is known regarding the association between frailty status and a patient’s hospitalization outcomes. Our study investigated whether frailty increases risk for readmission and inpatient mortality in RA patients.
Methods: Using the 2018 Nationwide Readmissions Database, we identified adult patients (age ≥18 years) admitted with a primary or secondary diagnosis of RA (using ICD 10 codes) between January to June 2018. Utilizing validated claim-based Hospital Frailty Score3, patients’ frailty risk score was calculated at the time of index admission and individuals were categorized into frail (score ≥ 5) and non-frail (score < 5) groups. Our primary outcome of interest was risk of readmission following discharge after index hospitalization. Secondary outcomes of interest included inpatient mortality, prolonged length of admission (≥ 7 days), mean days to readmission, and costs of hospitalization. We used descriptive statistics to compare patient demographics, admission characteristics, and hospital characteristics at index hospitalization in frail vs non-frail groups. Multivariable Cox proportional hazard analysis was performed to evaluate the independent effect of frailty on readmission after controlling for age, sex, household income, hospital characteristics (teaching status, capacity, location), and Elixhauser comorbidities index.
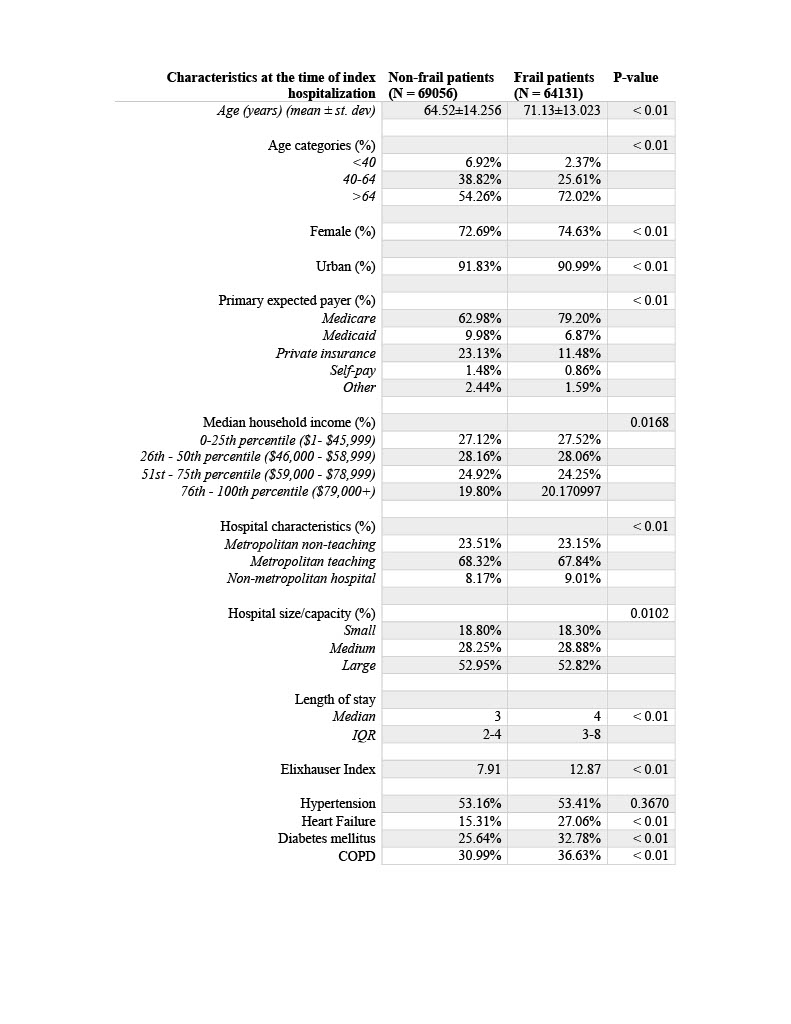
Results: 133,187 patients with RA met our inclusion criteria. Of these, 64,131 (48.15%) patients were categorized as frail, and 69,056 (51.85%) patients were non-frail. Frail patients were older, female, predominantly with Medicare coverage, and had higher Elixhauser comorbidity index (Table 1). Frail patients had a higher rate of readmission (56.60%) compared to the non-frail group (30.61%). After readmission, frail patients also had significantly higher inpatient mortality compared to non-frail patients (3.36% vs 0.39%, p < 0.005) and a longer length of stay (7.82% vs 26.24%, p < 0.005) (Table 2). On multivariate analysis, frailty was independently associated with a 9% increased risk of readmissions (adjusted hazard ratio, 1.09; 95% confidence interval, 1.08 – 1.11) (Table 3).
Conclusion: Frailty is associated with a higher risk of readmissions in patients with RA. In addition, frail patients with RA have higher likelihood for poorer outcomes after hospitalization (such as increased inpatient mortality) relative to non-frail patients. These findings are crucial in identifying hospitalized patients with RA who are at a higher risk of worse outcomes. Future studies should explore modifiable factors to mitigate these risks.
References:
1. van Onna M, et al. PMID: 35314796.
2. Hanlon P, et al. PMID: 35292529.
3. Gilbert T, et al. PMID: 29706364
.
To cite this abstract in AMA style:
Tahir W, Rosli Y, Leung C, Wysham K, Lee J, Goulabchand R, Makris U, Singh S, Singh N. Frailty Is Associated with Higher Risk of Readmission in Patients with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/frailty-is-associated-with-higher-risk-of-readmission-in-patients-with-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/frailty-is-associated-with-higher-risk-of-readmission-in-patients-with-rheumatoid-arthritis/